Correlation of nighttime fasting duration with cognitive decline in older adults: a cross-sectional study based on NHANES 2011-2014
DOI:
https://doi.org/10.71321/pzxtk440Keywords:
Cognitive Function, Nutrition Examination Survey, Nighttime Fasting Duration, US National HealthAbstract
Background: Cognitive dysfunction is a significant health challenge in the global elderly population, and its prevalence is associated with multiple factors, including modifiable lifestyle factors. The relationship between nighttime fasting duration, a potential lifestyle factor, and cognitive function has yet to be thoroughly investigated.
Objective: To investigate the association between nighttime fasting duration and cognitive function.
Methods: This cross-sectional study was based on data from the National Health and Nutrition Examination Survey (NHANES) from 2011 to 2014. Weighted multiple linear regression was utilized to examine the relationship between nighttime fasting duration and cognitive function, with additional curve fitting and inflection point analysis conducted to further elucidate this association
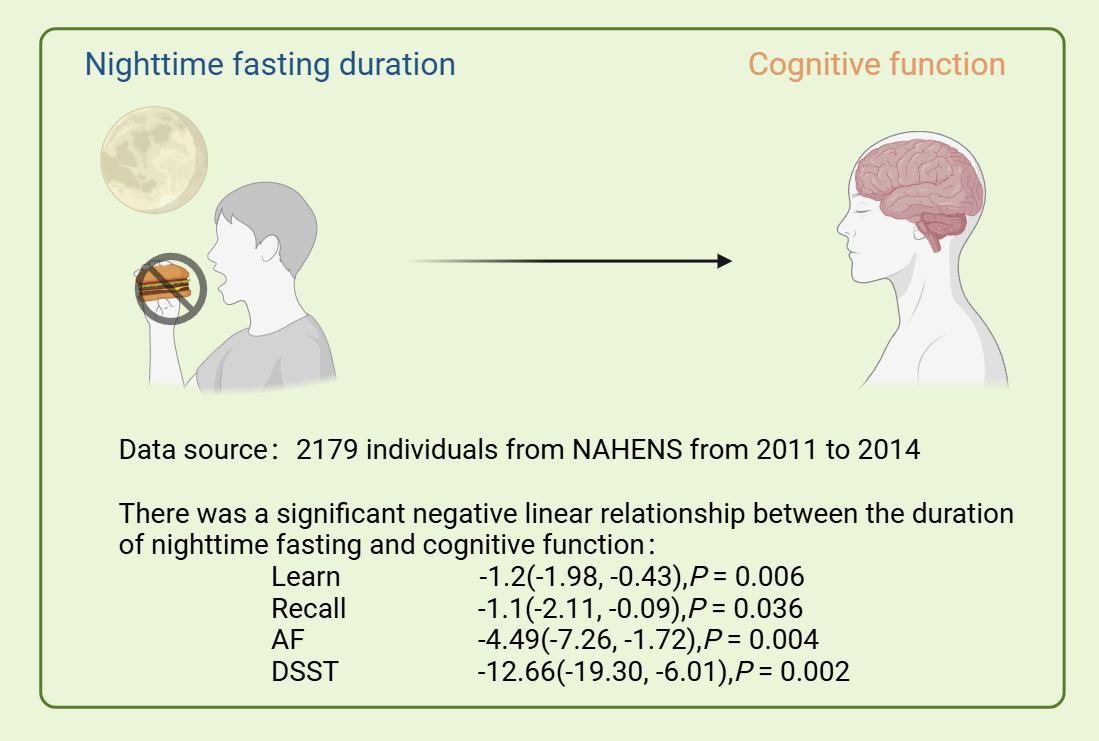
Results: There was a significant negative linear relationship between nighttime fasting duration and cognitive function (Learn: β = -1.2, 95% CI: -1.98, -0.43, P = 0.006; Recall: β = -1.1, 95% CI: -2.11, -0.09, P = 0.036; Animal Fluency: β = -4.49, 95% CI: -7.26, -1.72, P = 0.004; Digit Symbol Substitution Test: β = -12.66, 95% CI: -19.30, -6.01, P = 0.002). Subgroup analyses showed that this negative correlation was prevalent in most subgroups. Curve fitting revealed a linear relationship between nighttime fasting duration and cognitive function scores, but did not identify a significant inflection point.
Conclusions: Longer nighttime fasting times may be associated with cognitive decline, either as a continuous or categorical variable.
References
[1] Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement. 2013;9(1):63-75.e2.
[2] Zhao M, Chen Z, Xu T, Fan P, Tian F. Global prevalence of polypharmacy and potentially inappropriate medication in older patients with dementia: a systematic review and meta-analysis. Front Pharmacol. 2023;14:1221069.
[3] Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol. 2003;60(8):1119-22.
[4] Aibar-Almazán A, Voltes-Martínez A, Castellote-Caballero Y, Afanador-Restrepo DF, Carcelén-Fraile MDC, López-Ruiz E. Current Status of the Diagnosis and Management of Osteoporosis. Int J Mol Sci. 2022;23(16).
[5] Li X, Feng X, Sun X, Hou N, Han F, Liu Y. Global, regional, and national burden of Alzheimer's disease and other dementias, 1990-2019. Front Aging Neurosci. 2022;14:937486.
[6] Chu CQ, Yu LL, Qi GY, Mi YS, Wu WQ, Lee YK, et al. Can dietary patterns prevent cognitive impairment and reduce Alzheimer's disease risk: Exploring the underlying mechanisms of effects. Neurosci Biobehav Rev. 2022;135:104556.
[7] O'Leary J, Georgeaux-Healy C, Serpell L. The impact of continuous calorie restriction and fasting on cognition in adults without eating disorders. Nutr Rev. 2024.
[8] Alkurd R, Mahrous L, Zeb F, Khan MA, Alhaj H, Khraiwesh HM, et al. Effect of Calorie Restriction and Intermittent Fasting Regimens on Brain-Derived Neurotrophic Factor Levels and Cognitive Function in Humans: A Systematic Review. Medicina (Kaunas). 2024;60(1).
[9] Hofer SJ, Carmona-Gutierrez D, Mueller MI, Madeo F. The ups and downs of caloric restriction and fasting: from molecular effects to clinical application. EMBO Mol Med. 2022;14(1):e14418.
[10] Vasim I, Majeed CN, DeBoer MD. Intermittent Fasting and Metabolic Health. Nutrients. 2022;14(3).
[11] Mattson MP, Longo VD, Harvie M. Impact of intermittent fasting on health and disease processes. Ageing Res Rev. 2017;39:46-58.
[12] Wahl D, Cogger VC, Solon-Biet SM, Waern RV, Gokarn R, Pulpitel T, et al. Nutritional strategies to optimise cognitive function in the aging brain. Ageing Res Rev. 2016;31:80-92.
[13] Anson RM, Guo Z, de Cabo R, Iyun T, Rios M, Hagepanos A, et al. Intermittent fasting dissociates beneficial effects of dietary restriction on glucose metabolism and neuronal resistance to injury from calorie intake. Proc Natl Acad Sci U S A. 2003;100(10):6216-20.
[14] Fu M, Lu S, Gong L, Zhou Y, Wei F, Duan Z, et al. Intermittent fasting shifts the diurnal transcriptome atlas of transcription factors. Mol Cell Biochem. 2024.
[15] Morris JC, Heyman A, Mohs RC, Hughes JP, van Belle G, Fillenbaum G, et al. The Consortium to Establish a Registry for Alzheimer's Disease (CERAD). Part I. Clinical and neuropsychological assessment of Alzheimer's disease. Neurology. 1989;39(9):1159-65.
[16] Lindenberger U. Human cognitive aging: corriger la fortune? Science. 2014;346(6209):572-8.
[17] Beeri MS, Schmeidler J, Sano M, Wang J, Lally R, Grossman H, et al. Age, gender, and education norms on the CERAD neuropsychological battery in the oldest old. Neurology. 2006;67(6):1006-10.
[18] Brody DJ, Kramarow EA, Taylor CA, McGuire LC. Cognitive Performance in Adults Aged 60 and Over: National Health and Nutrition Examination Survey, 2011-2014. Natl Health Stat Report. 2019(126):1-23.
[19] Jaeger J. Digit Symbol Substitution Test: The Case for Sensitivity Over Specificity in Neuropsychological Testing. J Clin Psychopharmacol. 2018;38(5):513-9.
[20] Sotaniemi M, Pulliainen V, Hokkanen L, Pirttilä T, Hallikainen I, Soininen H, et al. CERAD-neuropsychological battery in screening mild Alzheimer's disease. Acta Neurol Scand. 2012;125(1):16-23.
[21] Tang H, Zhang X, Luo N, Huang J, Zhu Y. Association of Dietary Live Microbes and Nondietary Prebiotic/Probiotic Intake With Cognitive Function in Older Adults: Evidence From NHANES. J Gerontol A Biol Sci Med Sci. 2024;79(2).
[22] Chen L, Zou L, Chen J, Wang Y, Liu D, Yin L, et al. Association between cognitive function and body composition in older adults: data from NHANES (1999-2002). Front Aging Neurosci. 2024;16:1372583.
[23] Wilson RS, Mendes De Leon CF, Barnes LL, Schneider JA, Bienias JL, Evans DA, et al. Participation in cognitively stimulating activities and risk of incident Alzheimer disease. Jama. 2002;287(6):742-8.
[24] Mao J, Hu H, Zhao Y, Zhou M, Yang X. Association Between Composite Dietary Antioxidant Index and Cognitive Function Among Aging Americans from NHANES 2011-2014. J Alzheimers Dis. 2024;98(4):1377-89.
[25] St-Onge MP, Ard J, Baskin ML, Chiuve SE, Johnson HM, Kris-Etherton P, et al. Meal Timing and Frequency: Implications for Cardiovascular Disease Prevention: A Scientific Statement From the American Heart Association. Circulation. 2017;135(9):e96-e121.
[26] Cheng W, Meng X, Gao J, Jiang W, Sun X, Li Y, et al. Relationship between circadian eating behavior (daily eating frequency and nighttime fasting duration) and cardiovascular mortality. Int J Behav Nutr Phys Act. 2024;21(1):22.
[27] Makarem N, Sears DD, St-Onge MP, Zuraikat FM, Gallo LC, Talavera GA, et al. Habitual Nightly Fasting Duration, Eating Timing, and Eating Frequency are Associated with Cardiometabolic Risk in Women. Nutrients. 2020;12(10).
[28] Rahman HH, Niemann D, Munson-McGee SH. Association of albumin to creatinine ratio with urinary arsenic and metal exposure: evidence from NHANES 2015-2016. Int Urol Nephrol. 2022;54(6):1343-53.
[29] Arı E, Köseoğlu H, Eroğlu T. Predictive value of SIRI and SII for metastases in RCC: a prospective clinical study. BMC Urol. 2024;24(1):14.
[30] Zhang H, Liu X, Wang X, Jiang Y. Association of two novel systemic inflammatory biomarkers and frailty based on NHANES 2007-2018. Front Public Health. 2024;12:1377408.
[31] Gudden J, Arias Vasquez A, Bloemendaal M. The Effects of Intermittent Fasting on Brain and Cognitive Function. Nutrients. 2021;13(9).
[32] Serger E, Luengo-Gutierrez L, Chadwick JS, Kong G, Zhou L, Crawford G, et al. The gut metabolite indole-3 propionate promotes nerve regeneration and repair. Nature. 2022;607(7919):585-92.
[33] Wang Y, Liang J, Xu B, Yang J, Wu Z, Cheng L. TrkB/BDNF signaling pathway and its small molecular agonists in CNS injury. Life sciences. 2024;336:122282.
[34] Li ST, Dai Q, Zhang SX, Liu YJ, Yu QQ, Tan F, et al. Ulinastatin attenuates LPS-induced inflammation in mouse macrophage RAW264.7 cells by inhibiting the JNK/NF-κB signaling pathway and activating the PI3K/Akt/Nrf2 pathway. Acta pharmacologica Sinica. 2018;39(8):1294-304.
[35] Wang L, Wang Q, Wang X, Yang C, Wang X, Liu H, et al. Intermittent fasting alleviates postoperative cognitive dysfunction by reducing neuroinflammation in aged mice. Brain research bulletin. 2024;216:111034.
[36] Chechko N, Vocke S, Habel U, Toygar T, Kuckartz L, Berthold-Losleben M, et al. Effects of overnight fasting on working memory-related brain network: an fMRI study. Human brain mapping. 2015;36(3):839-51.
[37] Ha K, Song Y. Associations of Meal Timing and Frequency with Obesity and Metabolic Syndrome among Korean Adults. Nutrients. 2019;11(10).
[38] Wang J, Rang Y, Liu C. Effects of Caloric Restriction and Intermittent Fasting and Their Combined Exercise on Cognitive Functioning: A Review. Current nutrition reports. 2024;13(4):691-700.
[39] Farese RV, Kindy MA, Sajan MP. Atypical Protein Kinase C Hyperactivity in Insulin-Resistant and Insulin-Sensitive Forms of Alzheimer’s Disease: A Potential Therapeutic Target. In: Huang X, editor. Alzheimer’s Disease: Drug Discovery. Brisbane (AU): Exon Publications; 2020.
[40] Cerqueira FM, da Cunha FM, Caldeira da Silva CC, Chausse B, Romano RL, Garcia CC, et al. Long-term intermittent feeding, but not caloric restriction, leads to redox imbalance, insulin receptor nitration, and glucose intolerance. Free Radic Biol Med. 2011;51(7):1454-60.
[41] Chen W, Cai W, Hoover B, Kahn CR. Insulin action in the brain: cell types, circuits, and diseases. Trends Neurosci. 2022;45(5):384-400.
[42] Hamzé R, Delangre E, Tolu S, Moreau M, Janel N, Bailbé D, et al. Type 2 Diabetes Mellitus and Alzheimer's Disease: Shared Molecular Mechanisms and Potential Common Therapeutic Targets. Int J Mol Sci. 2022;23(23).
[43] Fontana L, Meyer TE, Klein S, Holloszy JO. Long-term calorie restriction is highly effective in reducing the risk for atherosclerosis in humans. Proc Natl Acad Sci U S A. 2004;101(17):6659-63.
[44] McGrattan AM, McGuinness B, McKinley MC, Kee F, Passmore P, Woodside JV, et al. Diet and Inflammation in Cognitive Ageing and Alzheimer's Disease. Curr Nutr Rep. 2019;8(2):53-65.
[45] Tan BL, Norhaizan ME. Effect of High-Fat Diets on Oxidative Stress, Cellular Inflammatory Response and Cognitive Function. Nutrients. 2019;11(11).
[46] Furtado A, Costa D, Lemos MC, Cavaco JE, Santos CRA, Quintela T. The impact of biological clock and sex hormones on the risk of disease. Adv Protein Chem Struct Biol. 2023;137:39-81.
[47] Shelly S, Ramon-Gonen R, Paul P, Klein CJ, Klang E, Rahman N, et al. Nerve Conduction Differences in a Large Clinical Population: The Role of Age and Sex. J Neuromuscul Dis. 2023;10(5):925-35.
[48] Harriden B, D'Cunha NM, Kellett J, Isbel S, Panagiotakos DB, Naumovski N. Are dietary patterns becoming more processed? The effects of different dietary patterns on cognition: A review. Nutr Health. 2022;28(3):341-56.
Type
Published
Data Availability Statement
Additional data related to this paper may be requested from the authors.
Issue
Section
License
Copyright (c) 2025 Brain Conflux

This work is licensed under a Creative Commons Attribution 4.0 International License.







