Surgical Outcomes and Complications of Adult Thalamic Gliomas:A Systematic Review and Meta-Analysis
DOI:
https://doi.org/10.71321/jz58zk51Keywords:
Thalamic gliomas, Surgical resection, Postoperative complications, Adjuvant therapy, Overall survivalAbstract
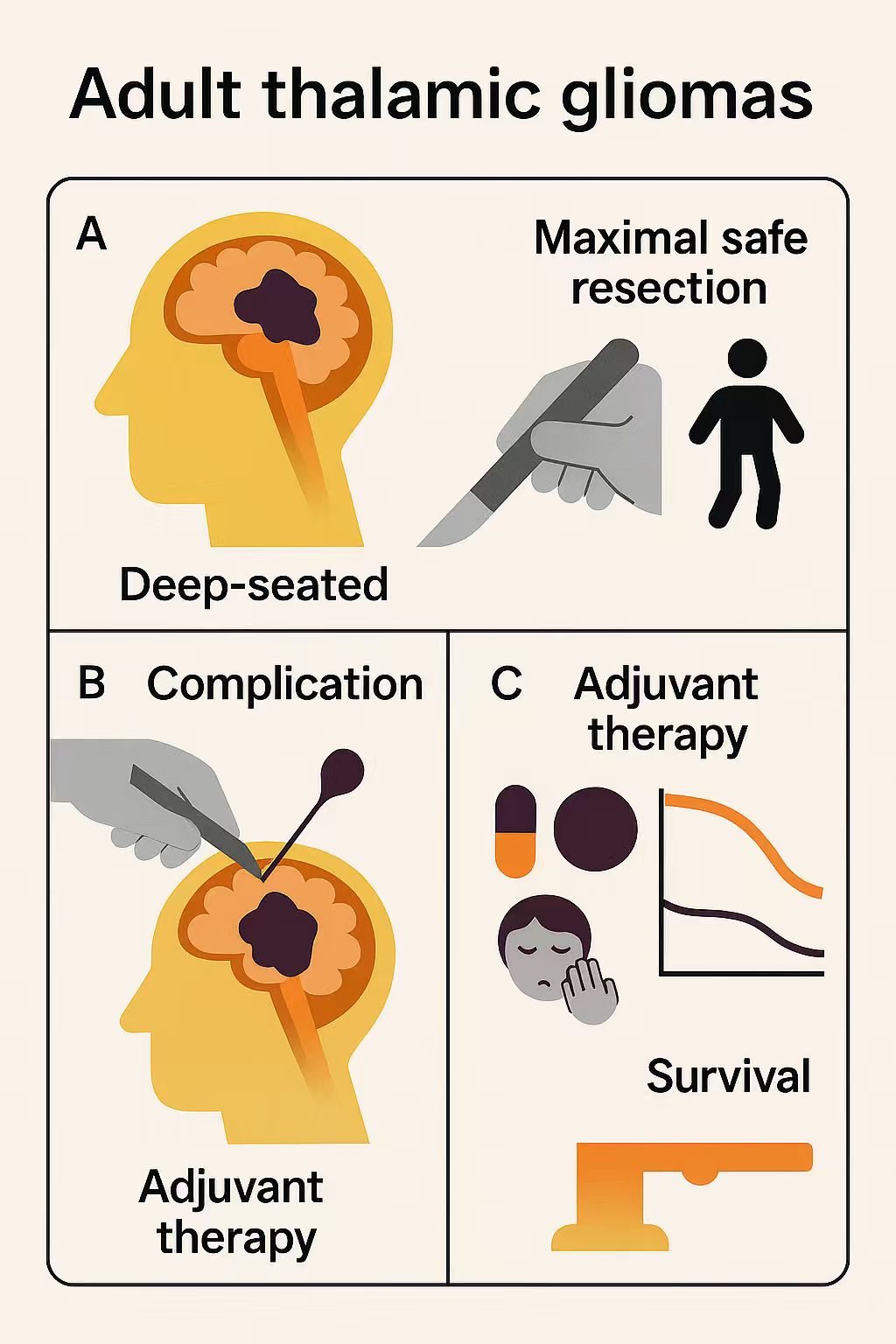
Objective: This systematic review and meta-analysis evaluated surgical outcomes, complications, and survival in adult thalamic glioma patients to inform optimal surgical and adjuvant treatment strategies.
Methods: We searched PubMed, Web of Science, and Embase up to July 10, 2025, analyzing 15 studies with 695 adults. Data included patient characteristics, surgical approaches (lateral, medial, posterior), extent of resection (EOR, gross total/subtotal resection [GTR/STR]), or partial resection [PR]), complications, and overall survival (OS). Cox proportional hazards models assessed survival factors (p<0.05).
Results: High-grade gliomas (HGGs) accounted for the majority (77.8%), and GTR/STR was achieved in 86.1% of cases, primarily through a lateral-related surgical approach (51.8%). Common postoperative complications were movement disorders (29%), infection/fever (25%), and sensory disorders (13%). In the pooled cohort consisting of 103 patients, median OS was 16 months for HGGs and 23 months for low-grade gliomas (LGGs). Multivariate Cox analysis confirmed prolonged OS in LGGs (hazard ratios [HRs]: 0.34, p = 0.005) and with adjuvant therapies (chemotherapy: HR 0.19, p=0.025; radiotherapy: HR 0.10, p=0.002; radiochemotherapy: HR 0.13, p=0.003).
Conclusion: Maximal safe resection with adjuvant therapies enhances survival in thalamic gliomas, despite high complication rates. Tailored surgical strategies and molecular profiling, are essential to optimize outcomes and guide targeted therapies.
References
[1] Sun Q, Zhao X, Gandhi S, Tayebi Meybodi A, Belykh E, Valli D, et al. (2020). Quantitative analysis of ipsilateral and contralateral supracerebellar infratentorial and occipital transtentorial approaches to the cisternal pulvinar: laboratory anatomical investigation. J Neurosurg, 133(4), 1172-1181. https://doi.org/10.3171/2019.4.Jns19351
[2] Puget S, Crimmins DW, Garnett MR, Grill J, Oliveira R, Boddaert N, et al. (2007). Thalamic tumors in children: a reappraisal. J Neurosurg, 106(5 Suppl), 354-362. https://doi.org/10.3171/ped.2007.106.5.354
[3] Solomon DA, Wood MD, Tihan T, Bollen AW, Gupta N, Phillips JJ, et al. (2016). Diffuse Midline Gliomas with Histone H3-K27M Mutation: A Series of 47 Cases Assessing the Spectrum of Morphologic Variation and Associated Genetic Alterations. Brain Pathol, 26(5), 569-580. https://doi.org/10.1111/bpa.12336
[4] Louis DN, Perry A, Wesseling P, Brat DJ, Cree IA, Figarella-Branger D, et al. (2021). The 2021 WHO Classification of Tumors of the Central Nervous System: a summary. Neuro Oncol, 23(8), 1231-1251. https://doi.org/10.1093/neuonc/noab106
[5] Castel D, Philippe C, Kergrohen T, Sill M, Merlevede J, Barret E, et al. (2018). Transcriptomic and epigenetic profiling of 'diffuse midline gliomas, H3 K27M-mutant' discriminate two subgroups based on the type of histone H3 mutated and not supratentorial or infratentorial location. Acta Neuropathol Commun, 6(1), 117. https://doi.org/10.1186/s40478-018-0614-1
[6] Albright AL. (2004). Feasibility and advisability of resections of thalamic tumors in pediatric patients. J Neurosurg, 100(5 Suppl Pediatrics), 468-472. https://doi.org/10.3171/ped.2004.100.5.0468
[7] Gambarin M, Malgrati T, Di Censo R, Modenese A, Balestro G, Muti G, et al. (2024). An Overview of Reviews on Predictors of Neurorehabilitation in Surgical or Non-Surgical Patients with Brain Tumours. Life (Basel), 14(11). https://doi.org/10.3390/life14111377
[8] Palmisciano P, Ferini G, Watanabe G, Ogasawara C, Lesha E, Bin-Alamer O, et al. (2022). Gliomas Infiltrating the Corpus Callosum: A Systematic Review of the Literature. Cancers (Basel), 14(10). https://doi.org/10.3390/cancers14102507
[9] Liu Y, Zhang Y, Hua W, Li Z, Wu B, & Liu W. (2019). Clinical and Molecular Characteristics of Thalamic Gliomas: Retrospective Report of 26 Cases. World Neurosurg, 126, e1169-e1182. https://doi.org/10.1016/j.wneu.2019.03.061
[10] Toader C, Radoi MP, Dumitru A, Glavan LA, Covache-Busuioc RA, Popa AA, et al. (2024). High-Grade Thalamic Glioma: Case Report with Literature Review. Medicina (Kaunas), 60(10). https://doi.org/10.3390/medicina60101667
[11] Steiger HJ, Götz C, Schmid-Elsaesser R, & Stummer W. (2000). Thalamic astrocytomas: surgical anatomy and results of a pilot series using maximum microsurgical removal. Acta Neurochir (Wien), 142(12), 1327-1336; discussion 1336-1327. https://doi.org/10.1007/s007010070001
[12] Vadhavekar NH, Sabzvari T, Laguardia S, Sheik T, Prakash V, Gupta A, et al. (2024). Advancements in Imaging and Neurosurgical Techniques for Brain Tumor Resection: A Comprehensive Review. Cureus, 16(10), e72745. https://doi.org/10.7759/cureus.72745
[13] Cinalli G, Aguirre DT, Mirone G, Ruggiero C, Cascone D, Quaglietta L, et al. (2018). Surgical treatment of thalamic tumors in children. J Neurosurg Pediatr, 21(3), 247-257. https://doi.org/10.3171/2017.7.PEDS16463
[14] Sai Kiran NA, Thakar S, Dadlani R, Mohan D, Furtado SV, Ghosal N, et al. (2013). Surgical management of thalamic gliomas: case selection, technical considerations, and review of literature. Neurosurg Rev, 36(3), 383-393. https://doi.org/10.1007/s10143-013-0452-3
[15] Lim J, Park Y, Ahn JW, Hwang SJ, Kwon H, Sung KS, et al. (2021). Maximal surgical resection and adjuvant surgical technique to prolong the survival of adult patients with thalamic glioblastoma. PLoS One, 16(2), e0244325. https://doi.org/10.1371/journal.pone.0244325
[16] Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj, 372, n71. https://doi.org/10.1136/bmj.n71
[17] Wu B, Tang C, Wang Y, Li Z, Hu S, Hua W, et al. (2018). High-grade thalamic gliomas: Microsurgical treatment and prognosis analysis. J Clin Neurosci, 49, 56-61. https://doi.org/10.1016/j.jocn.2017.12.008
[18] Saito R, Kumabe T, Kanamori M, Sonoda Y, & Tominaga T. (2017). Distant recurrences limit the survival of patients with thalamic high-grade gliomas after successful resection. Neurosurg Rev, 40(3), 469-477. https://doi.org/10.1007/s10143-016-0804-x
[19] Huang J, Li HY, Xu P, Ren XH, & Lin S. (2025). Effects of Surgical Ventricular Entry on Gliomas Invading the Thalamus: Clinical Outcomes and Economic Burdens. World Neurosurg, 196, 123731. https://doi.org/10.1016/j.wneu.2025.123731
[20] Li Z, Wu H, Wu B, Lyu J, Liu Y, Tang C, et al. (2020). Long term follow-up and outcomes in adult patients with thalamic gliomas. Clin Neurol Neurosurg, 195, 105888. https://doi.org/10.1016/j.clineuro.2020.105888
[21] Niu X, Wang T, Zhou X, Yang Y, Wang X, Zhang H, et al. (2020). Surgical treatment and survival outcome of patients with adult thalamic glioma: a single institution experience of 8 years. J Neurooncol, 147(2), 377-386. https://doi.org/10.1007/s11060-020-03430-x
[22] Que T, Li Z, Zheng H, Tan J-E, Yuan X, Yi G, et al. (2025). Classification of unilateral thalamic gliomas predicts tumor resection and patient's survival: a single center retrospective study [Article]. Journal of Neurosurgical Sciences, 69(1), 111-122. https://doi.org/10.23736/s0390-5616.22.05660-0
[23] Kis D, Mate A, Kincses ZT, Voros E, & Barzo P. (2014). The role of probabilistic tractography in the surgical treatment of thalamic gliomas. Neurosurgery, 10 Suppl 2, 262-272; discussion 272. https://doi.org/10.1227/NEU.0000000000000333
[24] Zhang P, Wang X, Ji N, Xie J, Han J, Ren X, et al. (2016). Clinical, radiological, and pathological features of 33 adult unilateral thalamic gliomas. World J Surg Oncol, 14, 78. https://doi.org/10.1186/s12957-016-0820-x
[25] Majchrzak K, Bobek-Billewicz B, Hebda A, Adamczyk P, Majchrzak H, & Ladzinski P. (2018). Surgical treatment of adult patients with thalamic tumors with the aid of tractography, fMRI, transcranial electrical stimulation and direct electrical stimulation of the subcortical white matter. Neurol Neurochir Pol, 52(6), 720-730. https://doi.org/10.1016/j.pjnns.2018.07.001
[26] Cao L, Li C, Zhang Y, & Gui S. (2015). Surgical resection of unilateral thalamic tumors in adults: approaches and outcomes. BMC Neurol, 15, 229. https://doi.org/10.1186/s12883-015-0487-x
[27] Guo Q, Hua W, Wu B, Li Z, Liu Y, Sun P, et al. (2020). Lateral or Medial Surgical Approaches for Thalamic Gliomas Resection? [Article]. World Neurosurgery, 136, E90-E107. https://doi.org/10.1016/j.wneu.2019.11.108
[28] Zheng X, Xu X, Zhang H, Wang Q, Ma X, Chen X, et al. (2016). A Preliminary Experience with Use of Intraoperative Magnetic Resonance Imaging in Thalamic Glioma Surgery: A Case Series of 38 Patients. World Neurosurg, 89, 434-441. https://doi.org/10.1016/j.wneu.2016.01.092
[29] Palmisciano P, El Ahmadieh TY, Haider AS, Bin Alamer O, Robertson FC, Plitt AR, et al. (2021). Thalamic gliomas in adults: a systematic review of clinical characteristics, treatment strategies, and survival outcomes. J Neurooncol, 155(3), 215-224. https://doi.org/10.1007/s11060-021-03898-1
[30] Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. (2016). The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol, 131(6), 803-820. https://doi.org/10.1007/s00401-016-1545-1
[31] Weller M, van den Bent M, Hopkins K, Tonn JC, Stupp R, Falini A, et al. (2014). EANO guideline for the diagnosis and treatment of anaplastic gliomas and glioblastoma. Lancet Oncol, 15(9), e395-403. https://doi.org/10.1016/s1470-2045(14)70011-7
[32] Gajjar A, Mahajan A, Bale T, Bowers DC, Canan L, Chi S, et al. (2025). Pediatric Central Nervous System Cancers, Version 2.2025, NCCN Clinical Practice Guidelines In Oncology. J Natl Compr Canc Netw, 23(3), 113-130. https://doi.org/10.6004/jnccn.2025.0012
[33] Gilbert MR, Dignam JJ, Armstrong TS, Wefel JS, Blumenthal DT, Vogelbaum MA, et al. (2014). A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Engl J Med, 370(8), 699-708. https://doi.org/10.1056/NEJMoa1308573
[34] Brat DJ, Verhaak RG, Aldape KD, Yung WK, Salama SR, Cooper LA, et al. (2015). Comprehensive, Integrative Genomic Analysis of Diffuse Lower-Grade Gliomas. N Engl J Med, 372(26), 2481-2498. https://doi.org/10.1056/NEJMoa1402121
[35] Mohammad F, Weissmann S, Leblanc B, Pandey DP, Højfeldt JW, Comet I, et al. (2017). EZH2 is a potential therapeutic target for H3K27M-mutant pediatric gliomas. Nat Med, 23(4), 483-492. https://doi.org/10.1038/nm.4293
[36] Yamagishi M, Kuze Y, Kobayashi S, Nakashima M, Morishima S, Kawamata T, et al. (2024). Mechanisms of action and resistance in histone methylation-targeted therapy. Nature, 627(8002), 221-228. https://doi.org/10.1038/s41586-024-07103-x
[37] Zhao L, Rao X, Huang C, Zheng R, Kong R, Chen Z, et al. (2023). Epigenetic reprogramming of carrier free photodynamic modulator to activate tumor immunotherapy by EZH2 inhibition. Biomaterials, 293, 121952. https://doi.org/10.1016/j.biomaterials.2022.121952
[38] Rangel-Castilla L, & Spetzler RF. (2015). The 6 thalamic regions: surgical approaches to thalamic cavernous malformations, operative results, and clinical outcomes. J Neurosurg, 123(3), 676-685. https://doi.org/10.3171/2014.11.JNS14381
[39] Sanai N, & Berger MS. (2008). Glioma extent of resection and its impact on patient outcome. Neurosurgery, 62(4), 753-764; discussion 264-756. https://doi.org/10.1227/01.neu.0000318159.21731.cf
[40] Brown TJ, Brennan MC, Li M, Church EW, Brandmeir NJ, Rakszawski KL, et al. (2016). Association of the Extent of Resection With Survival in Glioblastoma: A Systematic Review and Meta-analysis. JAMA Oncol, 2(11), 1460-1469. https://doi.org/10.1001/jamaoncol.2016.1373
[41] Bello L, Castellano A, Fava E, Casaceli G, Riva M, Scotti G, et al. (2010). Intraoperative use of diffusion tensor imaging fiber tractography and subcortical mapping for resection of gliomas: technical considerations. Neurosurg Focus, 28(2), E6. https://doi.org/10.3171/2009.12.FOCUS09240
[42] Nimsky C, Ganslandt O, & Fahlbusch R. (2007). Implementation of fiber tract navigation. Neurosurgery, 61(1 Suppl), 306-317; discussion 317-308. https://doi.org/10.1227/01.neu.0000279224.83998.7d
[43] Duffau H. (2012). The challenge to remove diffuse low-grade gliomas while preserving brain functions. Acta Neurochir (Wien), 154(4), 569-574. https://doi.org/10.1007/s00701-012-1275-7
[44] Gupta N, & Pandey S. (2018). Post-Thalamic Stroke Movement Disorders: A Systematic Review. Eur Neurol, 79(5-6), 303-314. https://doi.org/10.1159/000490070
[45] Picillo M, Paramanandam V, Morgante F, Algarni M, Olszewska DA, Munhoz RP, et al. (2019). Dystonia as complication of thalamic neurosurgery. Parkinsonism Relat Disord, 66, 232-236. https://doi.org/10.1016/j.parkreldis.2019.08.008
[46] Cheng H, Chen BP, Soleas IM, Ferko NC, Cameron CG, & Hinoul P. (2017). Prolonged Operative Duration Increases Risk of Surgical Site Infections: A Systematic Review. Surg Infect (Larchmt), 18(6), 722-735. https://doi.org/10.1089/sur.2017.089
[47] Yaşargil MG, Türe U, & Yaşargil DC. (2005). Surgical anatomy of supratentorial midline lesions. Neurosurg Focus, 18(6b), E1. https://doi.org/10.3171/foc.2005.18.6.14
[48] Hori T, Ishida A, Aihara Y, Matsuo S, Yoshimoto H, & Shiramizu H. (2018). Surgery of Critically Located Intracranial Gliomas. Prog Neurol Surg, 30, 186-203. https://doi.org/10.1159/000464396
[49] Karsy M, Guan J, Cohen AL, Jensen RL, & Colman H. (2017). New Molecular Considerations for Glioma: IDH, ATRX, BRAF, TERT, H3 K27M. Curr Neurol Neurosci Rep, 17(2), 19. https://doi.org/10.1007/s11910-017-0722-5
[50] Yan H, Parsons DW, Jin G, McLendon R, Rasheed BA, Yuan W, et al. (2009). IDH1 and IDH2 mutations in gliomas. N Engl J Med, 360(8), 765-773. https://doi.org/10.1056/NEJMoa0808710
[51] Wu JS, Zhou LF, Tang WJ, Mao Y, Hu J, Song YY, et al. (2007). Clinical evaluation and follow-up outcome of diffusion tensor imaging-based functional neuronavigation: a prospective, controlled study in patients with gliomas involving pyramidal tracts. Neurosurgery, 61(5), 935-948; discussion 948-939. https://doi.org/10.1227/01.neu.0000303189.80049.ab
[52] Kokkinos V, Chatzisotiriou A, & Seimenis I. (2023). Functional Magnetic Resonance Imaging and Diffusion Tensor Imaging-Tractography in Resective Brain Surgery: Lesion Coverage Strategies and Patient Outcomes. Brain Sci, 13(11). https://doi.org/10.3390/brainsci13111574
[53] Conti Nibali M, Rossi M, Sciortino T, Riva M, Gay LG, Pessina F, et al. (2019). Preoperative surgical planning of glioma: limitations and reliability of fMRI and DTI tractography. J Neurosurg Sci, 63(2), 127-134. https://doi.org/10.23736/S0390-5616.18.04597-6
[54] Nabors B, Portnow J, Hattangadi-Gluth J, & Horbinski C. (2023). NCCN CNS tumor guidelines update for 2023. Neuro Oncol, 25(12), 2114-2116. https://doi.org/10.1093/neuonc/noad169
Type
Published
Issue
Section
License
Copyright (c) 2025 Head and Neck Diseases Conflux

This work is licensed under a Creative Commons Attribution 4.0 International License.







