Clinical Analysis of Children with Mixed Macrolide-Resistant Mycoplasma Pneumoniae Infection
DOI:
https://doi.org/10.71321/3xpc7j52Keywords:
Mycoplasma pneumoniae, mixed infection, hospitalized childrenAbstract
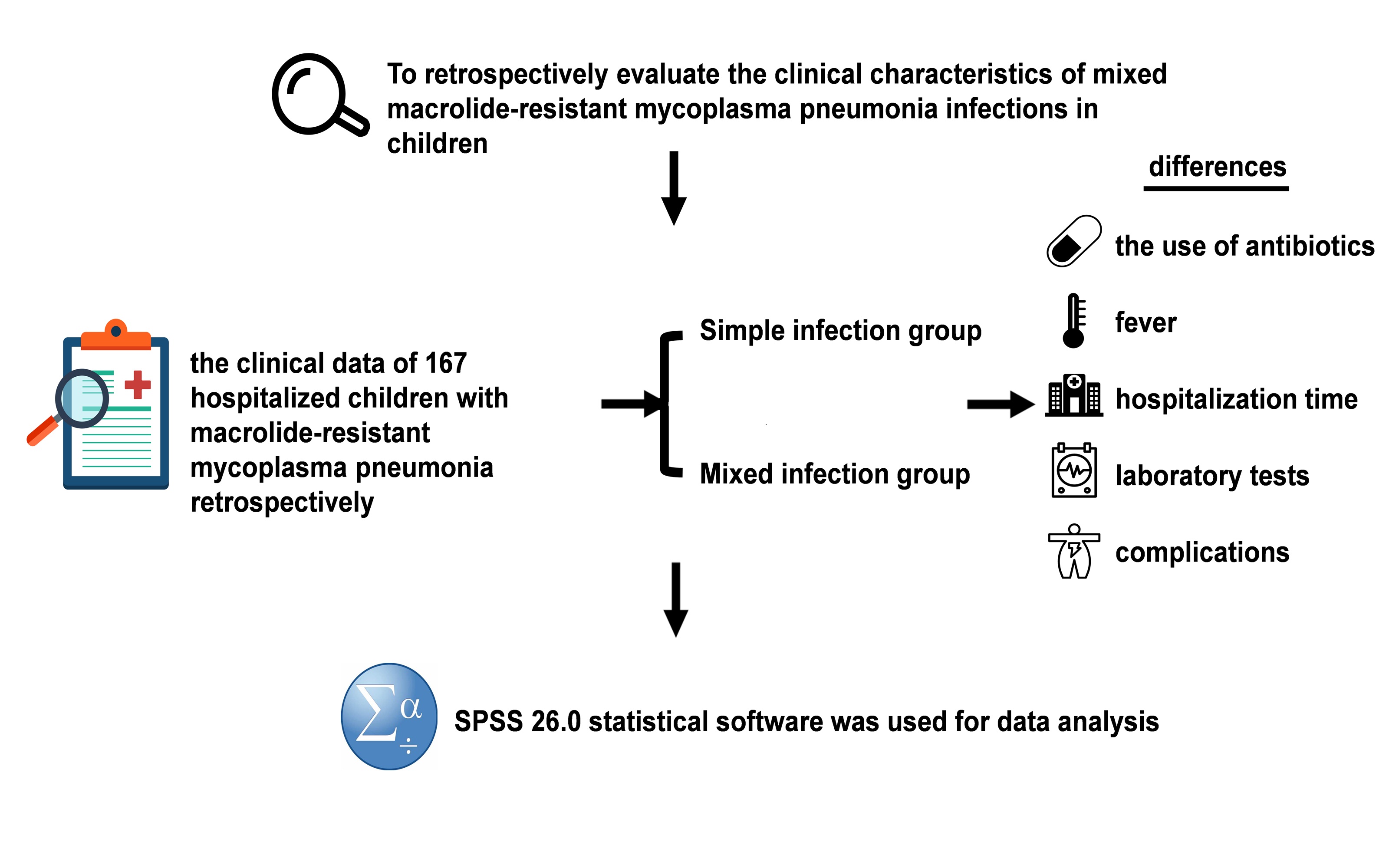
Purpose: To retrospectively evaluate the clinical characteristics of mixed macrolide-resistant mycoplasma pneumonia infections in children.
Methods: The study included 167 hospitalized children with macrolide-resistant mycoplasma pneumonia. We analyzed the children's clinical data retrospectively, and compared the differences in the use of antibiotics, fever, hospitalization time, laboratory tests and complications between the mixed infection group and the separately infected group before admission.
Results: Compared with the separately infected group, hospitalized children with mixed infection had a longer hospital stay, and there was a significant difference between the two (P<0.05); ALT, AST, LDH, CK, and PLT of children in the mixed infection group were significantly higher than those in the separately infected group (P<0.05); and the incidence of hepatic function impairment, cardiac enzyme profile abnormality, and pleural effusion in the children in the mixed infection group was higher than that in the separately infected group (P<0.01 ).
Conclusion: Patients with macrolide-resistant Mycoplasma pneumoniae pneumonia combined with mixed infections had prolonged hospital stays, increased systemic inflammatory response, and increased incidence of extrapulmonary complications compared with those with simple infections.
References
[1] Medjo B, Atanaskovic-Markovic M, Radic S, Nikolic D, Lukac M, Djukic S. Mycoplasma pneumoniae as a causative agent of community-acquired pneumonia in children: clinical features and laboratory diagnosis[J]. Italian Journal of Pediatrics, 2014, 40(1): 104. Doi: 10.1186/s13052-014-0104-4
[2] Zhao F, Li J, Liu J, Guan X, Gong J, Liu L, et al. Antimicrobial susceptibility and molecular characteristics of mycoplasma pneumoniae isolates across different regions of China[J]. Antimicrobial Resistance & Infection Control, 2019, 8: 143. Doi: 10.1186/s13756-019-0576-5
[3] Lee H, Yun K W, Lee H J, Choi E H. Antimicrobial therapy of macrolide-resistant mycoplasma pneumoniae pneumonia in children[J]. Expert Review of Anti-Infective Therapy, 2018, 16(1): 23-34. Doi: 10.1080/14787210.2018.1414599
[4] Norton S A. Diagnosing mycoplasma pneumoniae-induced rash and mucositis (MIRM) in the emergency room[J]. Journal of the American Academy of Dermatology, 2015, 73(2): e67. Doi: 10.1016/j.jaad.2015.03.060
[5] Scapini J P, Flynn L P, Sciacaluga S, Morales L, Cadario M E. Confirmed mycoplasma pneumoniae endocarditis[J]. Emerging Infectious Diseases, 2008, 14(10): 1664-1665. Doi:
[6] Kawai Y, Miyashita N, Kubo M, Akaike H, Kato A, Nishizawa Y, et al. Therapeutic efficacy of macrolides, minocycline, and tosufloxacin against macrolide-resistant mycoplasma pneumoniae in pediatric patients[J]. pneumoniae pneumonia in pediatric patients[J]. Antimicrobial Agents and Chemotherapy, 2013, 57(5): 2252-2258. Doi:
[7] Wang A, Wu Z, Huang Y, Zhou H, Wu L, Jia C P, et al. A 3D-printed microfluidic device for qPCR detection of macrolide-resistant mutations of mycoplasma pneumoniae[J]. Biosensors, 2021, 11(11): 427. Doi: 10.3390/bios11110427
[8] Li F, Zhang Y, Shi P, Cao L, Su L, Fu P, et al. Mycoplasma pneumoniae and adenovirus coinfection cause pediatric severe community-acquired pneumonia[J]. Microbiology Spectrum, 2022, 10(2): e0002622. Doi: 10.1128/spectrum.00026-22
[9] Sung M, Choi H J, Lee M H, Lee J Y, Kim H B, Ahn Y M, et al. Regional and annual patterns in respiratory virus co-infection etiologies and antibiotic prescriptions for pediatric mycoplasma pneumoniae pneumonia[J]. European Review for Medical and Pharmacological Sciences, 2022, 26(16): 5844-5856. Doi: 10.26355/eurrev_202208_29524
[10] Fan B E, Lim K G E, Chong V C L, Chan S S W, Ong K H, Kuperan P. COVID-19 and mycoplasma pneumoniae coinfection[J]. American Journal of Hematology, 2020, 95(6): 723-724. Doi: 10.1002/ajh.25785
[11] Zha L, Shen J, Tefsen B, Wang Y, Lu W, Xu Q. Clinical features and outcomes of adult COVID-19 patients co-infected with mycoplasma pneumoniae[J]. Journal of Infection, 2020, 81(3): e12-e15. Doi: 10.1016/j.jinf.2020.07.010
[12] Ni X. Community-acquired pneumonia diagnosis and treatment standard for children (2019 edition)[J]. Clinical and Education in Family Medicine, 2019, 17(9): 771-777. Doi: 10.13558/j.cnki.issn1672-3686.2019.09.002
[13] Matsuoka M, Narita M, Okazaki N, Ohya H, Yamazaki T, Ouchi K, et al. Characterization and molecular analysis of macrolide-resistant mycoplasma pneumoniae clinical isolates obtained in Japan[J]. Antimicrobial Agents and Chemotherapy, 2004, 48(12): 4624-4630. Doi: 10.1128/AAC.48.12.4624-4630.2004
[14] De Francesco M A, Poiesi C, Gargiulo F, Bonfanti C, Pollara P, Fiorentini S, et al. Co-infection of chlamydia pneumoniae and mycoplasma pneumoniae with SARS-CoV-2 is associated with more severe features[J]. Journal of Infection, 2021, 82(4): e4-e7. Doi: 10.1016/j.jinf.2021.01.009
[15] Xiong Y Z, He L M. Clinical analysis of infectious mononucleosis combined with Mycoplasma pneumoniae infection in children[J]. Journal of Nanchang University (Medical Edition), 2023, 63(5): 63-65, 74. Doi: 10.13764/j.cnki.ncdm.2023.05.011
[16] Shin S, Koo S, Yang Y J, Lim H J. Characteristics of the mycoplasma pneumoniae epidemic from 2019 to 2020 in korea: macrolide resistance and Co-infection trends[J]. Antibiotics (Basel, Switzerland), 2023, 12(11): 1623. Doi: 10.3390/antibiotics12111623
[17] Poddighe D. Extra-pulmonary diseases related to mycoplasma pneumoniae in children: recent insights into the pathogenesis[J]. Current Opinion in Rheumatology, 2018, 30(4): 380. Doi: 10.1097/BOR.0000000000000494
[18] Jiang Xingyuan, 2022, Study on Mycoplasma pneumoniae infection and drug-resistant mutation in children in Guangyuan area [D]. Chuanbei Medical College,2023. Doi: 10.27755/d.cnki.gcbyx.2023.000377
[19] Wu T. Study on the prevalence characteristics of Mycoplasma pneumoniae drug resistance genes and their correlation with genotypes in Yunnan [D]. Kunming University of Science and Technology,2023. Doi: 10.27200/d.cnki.gkmlu.2023.001981
[20] Chen Y, Zhang Y, Tang Q N, Shi H B. Efficacy of doxycycline therapy for macrolide-resistant mycoplasma pneumoniae pneumonia in children at different periods[J]. Italian Journal of Pediatrics, 2024, 50(1): 38. Doi: 10.1186/s13052-024-01615-y
[21] Luo X Q, Luo J, Wang C J, Luo Z X, Tian D Y, Xie X H. Clinical features of severe mycoplasma pneumoniae pneumonia with pulmonary complications in childhood: a retrospective study[J]. Pediatric Pulmonology, 2023, 58(10): 2815-2822. Doi: 10.1002/ppul.26593
[22] Fernald G W. Immunologic mechanisms suggested in the association of M. pneumoniae infection and extrapulmonary disease: a review[J]. Yale Journal of Biology and Medicine, 1983, 56(5-6): 475. PMID:6433568;PMCID:PMC2590510.
Type
Published
Data Availability Statement
All research data are available.
Issue
Section
License
Copyright (c) 2025 Life Conflux

This work is licensed under a Creative Commons Attribution 4.0 International License.







