Forearm necrotizing fasciitis caused by freshwater fish in an immunocompromised patient with rheumatoid arthritis for 20 years: a case report and review of the literature
DOI:
https://doi.org/10.71321/t6symt70Keywords:
Necrotizing fasciitis, Aeromonas sobria, Immunocompromised host, Septic shockAbstract
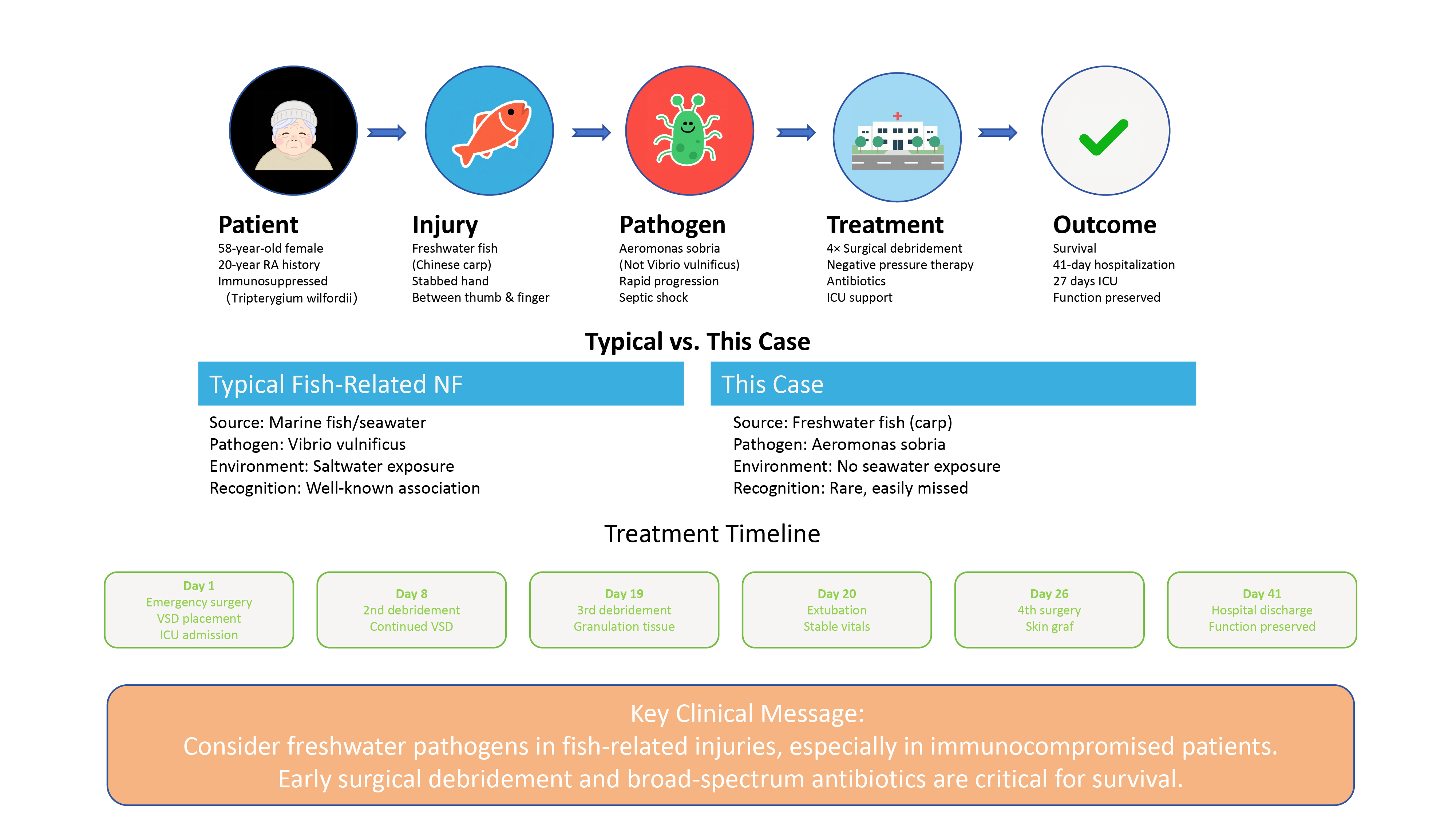
Necrotizing fasciitis (NF) is a life-threatening soft tissue infection typically associated with marine pathogens such as Vibrio vulnificus in cases involving fish-related injuries. This case report describes a rare instance of NF caused by Aeromonas sobria following a freshwater fish (Chinese carp) injury in a 58-year-old immunocompromised woman with a 20-year history of rheumatoid arthritis on long-term immunosuppressive therapy. The patient presented with rapid-onset swelling, pain, and septic shock, requiring intensive care, vasopressor support, and four surgical debridements with negative pressure wound therapy. Wound cultures confirmed Aeromonas sobria, contrasting with the more common marine-acquired Vibrio infections. Despite delayed diagnosis, aggressive multimodal management—including broad-spectrum antibiotics (piperacillin-tazobactam followed by meropenem) and repeated surgical interventions—resulted in survival after 41 days of hospitalization. This case highlights the importance of considering freshwater pathogens in NF, particularly in immunocompromised patients, and underscores the critical role of early surgical debridement and empiric antimicrobial coverage for atypical organisms. Clinicians should maintain a high suspicion for NF in fish-related injuries, even without marine exposure, to prevent fatal outcomes.
References
[1] Narendrakumar L, Gopinathan A, Sreekrishnan TP, Asokan A, Kumar A, Kumar G, et al. (2021). The bane of coastal marine environment: A fatal case of Vibrio vulnificus associated cellulitis and septicaemia. Indian J Med Microbiol, 39(3), 386-388. https://doi.org/10.1016/j.ijmmb.2021.05.016
[2] Coerdt KM, & Khachemoune A. (2021). Vibrio vulnificus: Review of Mild to Life-threatening Skin Infections. Cutis, 107(2), E12-e17. https://doi.org/10.12788/cutis.0183
[3] Spector CL, Hernandez J, Kiffin C, & Lee S. (2023). Fulminant Overwhelming Necrotizing Vibrio vulnificus Sepsis Secondary to Oyster Consumption. Am Surg, 89(9), 3896-3897. https://doi.org/10.1177/00031348231174013
[4] Leng F, Lin S, Wu W, Zhang J, Song J, & Zhong M. (2019). Epidemiology, pathogenetic mechanism, clinical characteristics, and treatment of Vibrio vulnificus infection: a case report and literature review. Eur J Clin Microbiol Infect Dis, 38(11), 1999-2004. https://doi.org/10.1007/s10096-019-03629-5
[5] Chang CY, Wu KH, Wu PH, Hung SK, Hsiao CT, Wu SR, et al. (2022). In-hospital mortality associated with necrotizing soft tissue infection due to Vibrio vulnificus: a matched-pair cohort study. World J Emerg Surg, 17(1), 28. https://doi.org/10.1186/s13017-022-00433-z
[6] Kattan AE, AlQahtani MS, Sultan FA, Alshaalan SF, Alkhars HF, Alblawi HK, et al. (2024). Necrotizing Fasciitis in a 9-year-old Girl. Plast Reconstr Surg Glob Open, 12(12), e6373. https://doi.org/10.1097/gox.0000000000006373
[7] Wong CH, Khin LW, Heng KS, Tan KC, & Low CO. (2004). The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: a tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care Med, 32(7), 1535-1541. https://doi.org/10.1097/01.ccm.0000129486.35458.7d
[8] Raveendranadh A, Prasad SS, & Viswanath V. (2024). Necrotizing fasciitis: treatment concepts & clinical outcomes - an institutional experience. BMC Surg, 24(1), 336. https://doi.org/10.1186/s12893-024-02638-2
[9] Chang CP, & Hsiao CT. (2023). Unreliable diagnostic accuracy of laboratory risk indicator for necrotizing fasciitis (LRINEC) score but good outcome predictor in necrotizing fasciitis due to Vibrio vulnificus : A retrospective and matched-pair study. Medicine (Baltimore), 102(27), e34207. https://doi.org/10.1097/md.0000000000034207
[10] Sahu KK, Mishra AK, & Lopez CA. (2020). Necrotizing fasciitis: challenges in diagnosis and management. Qjm, 113(3), 220-221. https://doi.org/10.1093/qjmed/hcz163
[11] Sartelli M, Viale P, Koike K, Pea F, Tumietto F, van Goor H, et al. (2011). WSES consensus conference: Guidelines for first-line management of intra-abdominal infections. World J Emerg Surg, 6, 2. https://doi.org/10.1186/1749-7922-6-2
[12] Naqvi GA, Malik SA, & Jan W. (2009). Necrotizing fasciitis of the lower extremity: a case report and current concept of diagnosis and management. Scand J Trauma Resusc Emerg Med, 17, 28. https://doi.org/10.1186/1757-7241-17-28
[13] Jones EJ, & Drew PJ. (2024). Assessment and management of necrotizing fasciitis. Br J Surg, 111(9). https://doi.org/10.1093/bjs/znae204
[14] Koppa BM, & Kelly CT. (2024). Point-of-care ultrasound in skin and soft tissue infections. J Hosp Med, 19(10), 938-944. https://doi.org/10.1002/jhm.13467
[15] Chaudhry AA, Baker KS, Gould ES, & Gupta R. (2015). Necrotizing fasciitis and its mimics: what radiologists need to know. AJR Am J Roentgenol, 204(1), 128-139. https://doi.org/10.2214/ajr.14.12676
[16] Hayeri MR, Ziai P, Shehata ML, Teytelboym OM, & Huang BK. (2016). Soft-Tissue Infections and Their Imaging Mimics: From Cellulitis to Necrotizing Fasciitis. Radiographics, 36(6), 1888-1910. https://doi.org/10.1148/rg.2016160068
[17] Tso DK, & Singh AK. (2018). Necrotizing fasciitis of the lower extremity: imaging pearls and pitfalls. Br J Radiol, 91(1088), 20180093. https://doi.org/10.1259/bjr.20180093
[18] Roje Z, Roje Z, Eterović D, Druzijanić N, Petrićević A, Roje T, et al. (2008). Influence of adjuvant hyperbaric oxygen therapy on short-term complications during surgical reconstruction of upper and lower extremity war injuries: retrospective cohort study. Croat Med J, 49(2), 224-232. https://doi.org/10.3325/cmj.2008.2.224
[19] Elliott DC, Kufera JA, & Myers RA. (1996). Necrotizing soft tissue infections. Risk factors for mortality and strategies for management. Ann Surg, 224(5), 672-683. https://doi.org/10.1097/00000658-199611000-00011
[20] Nordstrom NK, Miranda M, Seifarth FG, & Drews JD. (2024). Polymicrobial lower extremity necrotising fasciitis in a young toddler with sepsis. BMJ Case Rep, 17(11). https://doi.org/10.1136/bcr-2024-262142
[21] Merola R, Negri C, Merola A, Farina A, Orlando RA, Pasqualucci A, et al. (2024). Necrotizing Fasciitis and Streptococcal Toxic Shock Syndrome: A Case Report. Cureus, 16(11), e73917. https://doi.org/10.7759/cureus.73917
[22] Nazerani S, Maghari A, Kalantar Motamedi MH, Vahedian Ardakani J, Rashidian N, & Nazerani T. (2012). Necrotizing fasciitis of the upper extremity, case report and review of the literature. Trauma Mon, 17(2), 309-312. https://doi.org/10.5812/traumamon.6398
[23] Molewa MC, Ogonowski-Bizos A, Els M, Birtles CM, & Kolojane MC. (2024). The microbiological profile of necrotising fasciitis at a secondary level hospital in Gauteng. S Afr J Infect Dis, 39(1), 542. https://doi.org/10.4102/sajid.v39i1.542
[24] Guliyeva G, Huayllani MT, Sharma NT, & Janis JE. (2024). Practical Review of Necrotizing Fasciitis: Principles and Evidence-based Management. Plast Reconstr Surg Glob Open, 12(1), e5533. https://doi.org/10.1097/gox.0000000000005533
[25] Agarwal P, Kukrele R, & Sharma D. (2019). Vacuum assisted closure (VAC)/negative pressure wound therapy (NPWT) for difficult wounds: A review. J Clin Orthop Trauma, 10(5), 845-848. https://doi.org/10.1016/j.jcot.2019.06.015
[26] Morykwas MJ, Argenta LC, Shelton-Brown EI, & McGuirt W. (1997). Vacuum-assisted closure: a new method for wound control and treatment: animal studies and basic foundation. Ann Plast Surg, 38(6), 553-562. https://doi.org/10.1097/00000637-199706000-00001
[27] Naz F, Javaid RH, Almas D, Yousuf B, Noor S, & Awan A. (2024). COMPARISON OF NEGATIVE PRESSURE VACUUM THERAPY (NPWT) AND TIE OVER DRESSING IN HEALING SKIN GRAFTS. J Ayub Med Coll Abbottabad, 36(2), 355-358. https://doi.org/10.55519/jamc-02-12913
[28] Donoso-Samper A, Camacho-Obando D, Garzón S, & Gómez-Ortega V. (2024). Enhanced Negative Pressure Wound Therapy Shortens Hospital Stay for Major Burn Patients: Case Series. Plast Reconstr Surg Glob Open, 12(8), e6041. https://doi.org/10.1097/gox.0000000000006041
[29] Mankar S, Kawalkar A, Sakhare RH, & Suradkar P. (2024). Assessment of Vacuum-Assisted Closure (VAC) Therapy in Orthopaedic Infections. Cureus, 16(6), e63204. https://doi.org/10.7759/cureus.63204
[30] Faramarzi MR, Fatahi S, Rahimi K, Amini N, Imani A, & Babamiri B. (2024). Comprehensive infectious diabetic foot ulcer repair through multiple dressing methods, maggot therapy, and vacuum therapy after amputation: A case report study. Int J Surg Case Rep, 121, 109970. https://doi.org/10.1016/j.ijscr.2024.109970
[31] Sziklavari Z, Hammoudeh S, Petrone AM, Stange S, Orban K, Fekete JT, et al. (2025). Outcomes of Vacuum-Assisted Closure in Patients with Empyema Thoracis: A 10-Year Experience. Ann Thorac Surg, 119(6), 1206-1212. https://doi.org/10.1016/j.athoracsur.2024.08.003
[32] Buja Z. (2024). Lotus petal flap reconstruction of labia major and perineum after necrotizing fasciitis infection: A case report. SAGE Open Med Case Rep, 12, 2050313x241242593. https://doi.org/10.1177/2050313x241242593
[33] Mirzania D, Zhao Z, Kim DS, Aakalu VK, & Nelson CC. (2025). Umbilical Amniotic Tissue Graft as an Alternative Approach for Eyelid Reconstruction After Necrotizing Fasciitis Debridement. Ophthalmic Plast Reconstr Surg, 41(1), e18-e22. https://doi.org/10.1097/iop.0000000000002793
[34] Tobalem B, Conti E, Chatard M, Ghezal S, Soutif A, Merai R, et al. (2025). Reconstruction of trunk debridement after necrotizing fasciitis complicating varicella lesions with NovoSorb biodegradable temporizing matrix and skin graft: A pediatric case report. Ann Chir Plast Esthet, 70(2), 81-84. https://doi.org/10.1016/j.anplas.2024.12.001
[35] Roje Z, Roje Z, Matić D, Librenjak D, Dokuzović S, & Varvodić J. (2011). Necrotizing fasciitis: literature review of contemporary strategies for diagnosing and management with three case reports: torso, abdominal wall, upper and lower limbs. World J Emerg Surg, 6(1), 46. https://doi.org/10.1186/1749-7922-6-46
[36] Çelik M, Çiftçi MU, Çelik S, Öztürk V, Bayrak A, Duramaz A, et al. (2024). Can The Systemic Immune-Inflammation Index (SII) and Charlson Comorbidity Index (CCI) be used to predict mortality in patients with necrotizing fasciitis? Int Orthop, 48(7), 1707-1713. https://doi.org/10.1007/s00264-024-06190-9
[37] Kobayashi H, Otsubo T, Teraoka F, Ikeda K, Seike S, Takahashi E, et al. (2017). Involvement of the Arg566 residue of Aeromonas sobria serine protease in substrate specificity. PLoS One, 12(10), e0186392. https://doi.org/10.1371/journal.pone.0186392
[38] Hutchinson LE, Franke JD, & Mailey BA. (2021). Necrotizing fasciitis secondary to lake water inoculation with Aeromonas sobria: A case report. Medicine (Baltimore), 100(10), e24981. https://doi.org/10.1097/md.0000000000024981
[39] Al Nour AH, & Kothe S. (2024). [Fatal retroperitoneal necrotizing fasciitis due to Aeromonas caviae septicaemia]. Inn Med (Heidelb), 65(9), 952-954. https://doi.org/10.1007/s00108-024-01716-0
[40] Chang H, Hung YS, Shie SS, & Lin TL. (2012). Fulminant necrotizing fasciitis caused by Aeromonas sobria in neutropenic patients. Intern Med, 51(23), 3287-3290. https://doi.org/10.2169/internalmedicine.51.6281
[41] Das B, Ghafur A, S J, & Easow JM. (2022). A Case of Severe Aeromonas Bacteremia with Necrotizing Fasciitis of Lower Limb and Fournier ' s Gangrene in a Post-Allogenic Unrelated Hematopoietic Stem Cell Transplant Recipient. South Asian J Cancer, 11(3), 274-275. https://doi.org/10.1055/s-0042-1743164
[42] Tsai YH, Huang KC, Huang TJ, & Hsu RW. (2009). Case reports: fatal necrotizing fasciitis caused by Aeromonas sobria in two diabetic patients. Clin Orthop Relat Res, 467(3), 846-849. https://doi.org/10.1007/s11999-008-0504-0
Type
Published
Data Availability Statement
All data needed to evaluate the conclusions in the paper are present in the paper or the Supplementary Materials. Additional data related to this paper may be requested from the authors.
Issue
Section
License
Copyright (c) 2025 Life Conflux

This work is licensed under a Creative Commons Attribution 4.0 International License.







