Correlation Analysis between Spontaneous Nystagmus Characteristics and Semicircular Canal Dysfunction in Patients with Vestibular Neuritis: A Quantitative Study Using Electronystagmography and Video Head Impulse Test
DOI:
https://doi.org/10.71321/ceerva81Keywords:
vestibular neuritis, spontaneous nystagmus, video head impulse testAbstract
Objective: To compare the characteristics of spontaneous nystagmus (SN) in patients with vestibular neuritis (VN) at different disease stages and to investigate its correlation with semicircular canal dysfunction.
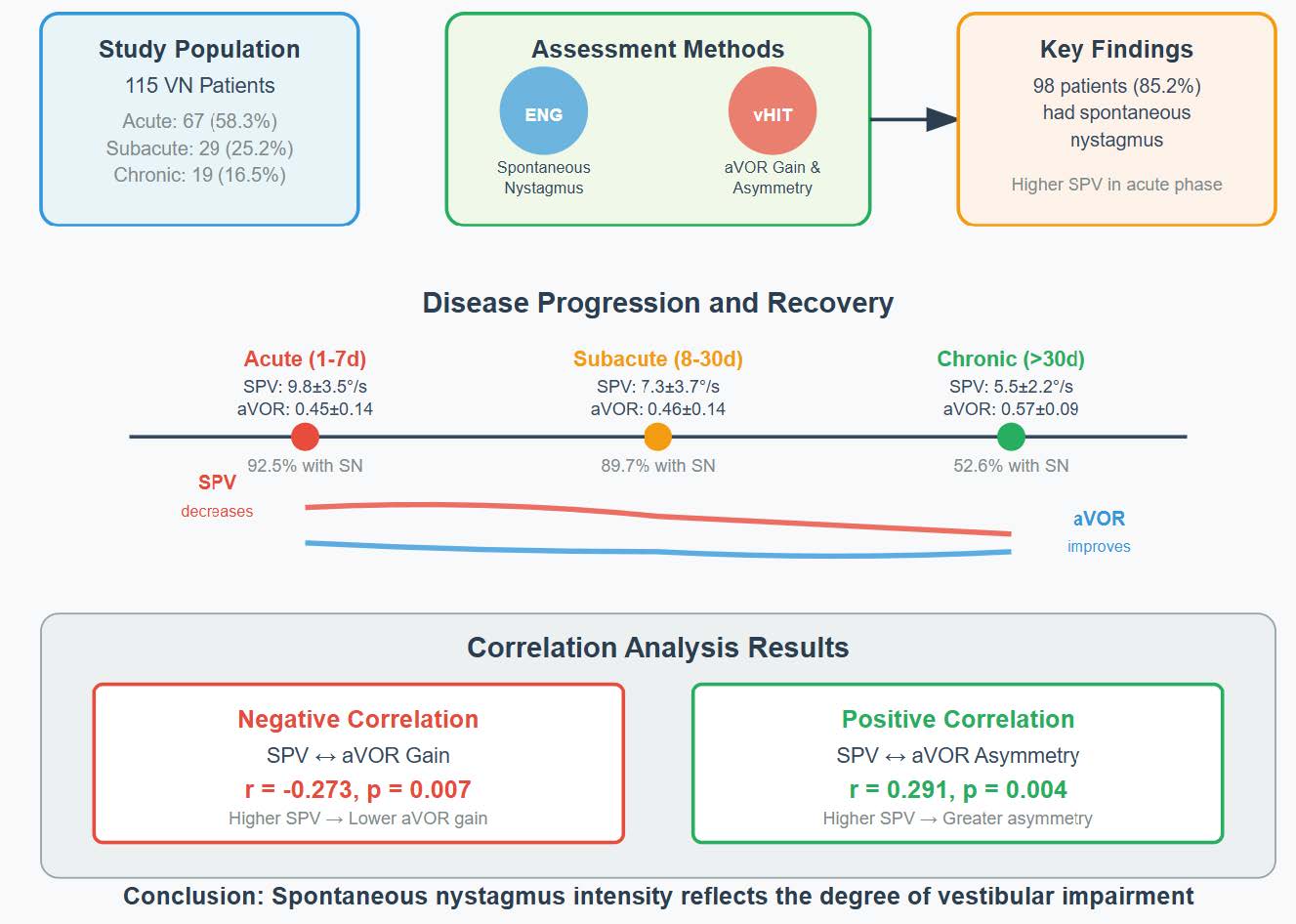
Methods: A total of 115 VN patients were enrolled, who were divided into acute phase (1 – 7 days), subacute phase (8 – 30 days) and chronic phase (>30 days) according to the course of disease. Quantitative assessment of SN was performed using electronystagmography (ENG), with particular focus on the slow phase velocity (SPV) in the horizontal plane. Simultaneously, vestibular-ocular reflex function was systematically evaluated through video head impulse test (vHIT), with quantitative measurements of angular vestibulo-ocular reflex (aVOR) gain and asymmetry of the affected semicircular canals.
Results: Among 115 patients, 67 (58.3%) were in acute phase, 29 (25.2%) in subacute phase and 19 (16.5%) in chronic phase. The mean age of patients in the acute phase was significantly lower than that in the chronic phase (p = 0.028), while there was no significant difference between the subacute phase and the other two groups. 98 patients (85.2%) had SN, 62 patients (92.5%) in acute phase, 26 patients (89.7%) in subacute phase and 10 patients (52.6%) in chronic phase. SPV in acute phase was significantly higher than that in subacute phase (p = 0.003) and chronic phase (p < 0.001), but there was no significant difference between chronic phase and subacute phase. In 112 patients with VN, the horizontal semicircular canals were affected, and the mean aVOR gain and asymmetry of the damaged side were 0.47 ± 0.14 and 0.35 ± 0.14, respectively. The aVOR gain of injured side in chronic phase was significantly higher than that in acute phase (p < 0.001) and subacute phase (p = 0.007), but there was no significant difference between acute phase and subacute phase (p = 0.950). The asymmetry in chronic phase was significantly lower than that in acute phase (p = 0.001) and subacute phase (p = 0.018), and there was no significant difference between acute phase and subacute phase (p = 0.312). SPV in horizontal component was negatively correlated with the aVOR gain of damaged horizontal semicircular canals (r = -0.273, p = 0.007), and positively correlated with aVOR asymmetry (r = 0.291, p = 0.004).
Conclusion: The existence of SN is helpful for diagnosis of VN, and its intensity can reflect the degree of vestibular impairment.
References
[1] Strupp M, Bisdorff A, Furman J, Hornibrook J, Jahn K, Maire R, Newman-Toker D, Magnusson M (2022) Acute unilateral vestibulopathy/vestibular neuritis: Diagnostic criteria. Journal of vestibular research : equilibrium & orientation 32(5):389-406. https://doi.org/10.3233/ves-220201
[2] Jasinska-Nowacka A, Niemczyk K (2024) Application of a Video Head Impulse Test in the Diagnosis of Vestibular Neuritis. Life (Basel) 14(6). https://doi.org/10.3390/life14060757
[3] Gianoli G, Goebel J, Mowry S, Poomipannit P (2005) Anatomic differences in the lateral vestibular nerve channels and their implications in vestibular neuritis. Otol Neurotol 26(3):489-494. https:// doi.org/10.1097/01.mao.0000169787.99835.9f
[4] Jacobson G, McCaslin D (2020) Vestibular Neuritis in Patients Among Different Age Groups: Clinical Features and Outcomes. J Am Acad Audiol 31(9):627-628. https://doi.org/10.1055/s-0041-1723789
[5] Scheltinga A, Honegger F, Timmermans DP, Allum JH (2016) The Effect of Age on Improvements in Vestibulo-Ocular Reflexes and Balance Control after Acute Unilateral Peripheral Vestibular Loss. Front Neurol 7:18. https://doi.org/10.3389/fneur.2016.00018
[6] Lacour M, Helmchen C, Vidal PP (2016) Vestibular compensation: the neuro-otologist's best friend. J Neurol 263 Suppl 1:S54-64. https://doi.org/10.1007/s00415-015-7903-4
[7] Darlington CL, Smith PF (2000) Molecular mechanisms of recovery from vestibular damage in mammals: recent advances. Prog Neurobiol 62(3):313-325. https://doi.org/10.1016/s0301-0082(00)00002-2
[8] Lacour M, Tighilet B (2010) Plastic events in the vestibular nuclei during vestibular compensation: the brain orchestration of a "deafferentation" code. Restor Neurol Neurosci 28(1):19-35. https://doi.org/10.3233/rnn-2010-0509
[9] Borel L, Lopez C, Péruch P, Lacour M (2008) Vestibular syndrome: a change in internal spatial representation. Neurophysiol Clin 38(6):375-389. https://doi.org/10.1016/j.neucli.2008.09.002
[10] Matsuzaki M, Kamei T (1995) Stage-assessment of the progress of continuous vertigo of peripheral origin by means of spontaneous and head-shaking nystagmus findings. Acta Otolaryngol Suppl 519:188-190. https://doi.org/10.3109/00016489509121900
[11] Robinson DA, Zee DS, Hain TC, Holmes A, Rosenberg LF (1984) Alexander's law: its behavior and origin in the human vestibulo-ocular reflex. Ann Neurol 16(6):714-722. https://doi.org/10.1002/ana.410160614
[12] Choi KD, Oh SY, Kim HJ, Koo JW, Cho BM, Kim JS (2007) Recovery of vestibular imbalances after vestibular neuritis. The Laryngoscope 117(7):1307-1312. https://doi.org/10.1097/MLG.0b013e31805c08ac
[13] Bergenius J, Perols O (1999) Vestibular neuritis: a follow-up study. Acta Otolaryngol 119(8):895-899. https://doi.org/10.1080/00016489950180243
[14] Zhang X, Deng Q, Liu Y, Li S, Wen C, Liu Q, Huang X, Wang W, Chen T (2023) Characteristics of spontaneous nystagmus and its correlation to video head impulse test findings in vestibular neuritis. Front Neurosci 17:1243720. https://doi.org/10.3389/fnins.2023.1243720
Type
Published
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Issue
Section
License
Copyright (c) 2025 Life Conflux

This work is licensed under a Creative Commons Attribution 4.0 International License.







