Headache mechanisms: what we still do not know
DOI:
https://doi.org/10.71321/h9jhnr48Keywords:
Migraine, Cluster headache, Tension-type headache, Calcitonin gene-related peptide, Pituitary adenylate cyclase-activating polypeptideAbstract
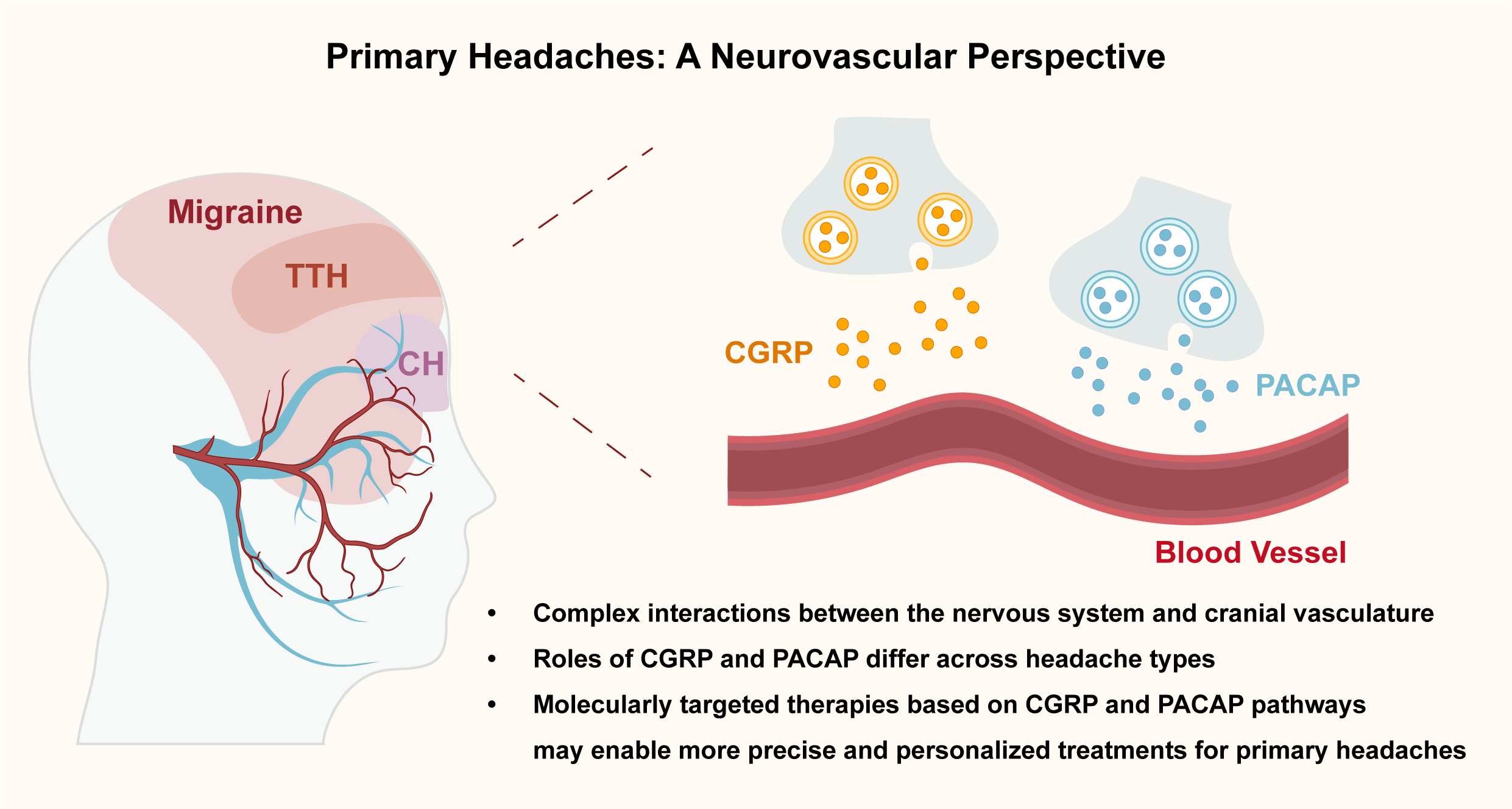
Primary headaches such as migraine, cluster headache (CH), and tension-type headache (TTH) are highly prevalent neurological disorders with complex and heterogeneous pathophysiology. Traditionally attributed to either vascular or neuronal origins, current evidence supports a neurovascular model involving dynamic interactions between the nervous system and cranial. This Perspective examines the role of two key neuropeptides – calcitonin gene-related peptide (CGRP) and pituitary adenylate cyclase-activating polypeptide (PACAP) – in the generation of primary headaches. CGRP is a validated target in migraine, but its clinical utility is limited by biomarker instability and a significant proportion of non-responders. PACAP is emerging as a complementary target, though its receptor mechanisms remain incompletely understood. While neither CGRP nor PACAP appear to play a major role in TTH, their contribution to migraine and CH highlights the need for precision approaches based on molecular endophenotypes. Understanding these mechanisms may inform the development of more effective, personalized headache treatments.
References
[1] Waliszewska-Prosół M, Montisano DA, Antolak M, Bighiani F, Cammarota F, Cetta I, et al. (2024). The impact of primary headaches on disability outcomes: a literature review and meta-analysis to inform future iterations of the Global Burden of Disease study. J Headache Pain. 2024;25(1):27. https://doi.org/10.1186/s10194-024-01735-0.
[2] Moskowitz MA. (2007). Pathophysiology of headache—past and present. Headache. 2007;47 Suppl 1:S58-63. https://doi.org/10.1111/j.1526-4610.2007.00678.x.
[3] Ashina M, Hansen JM, Do TP, Melo-Carrillo A, Burstein R, Moskowitz MA. (2019). Migraine and the trigeminovascular system—40 years and counting. Lancet Neurol. 2019;18(8):795-804. https://doi.org/10.1016/S1474-4422(19)30185-1.
[4] Guo S, Jansen-Olesen I, Olesen J, Christensen SL. (2023). Role of PACAP in migraine: An alternative to CGRP? Neurobiol Dis. 2023;176:105946. https://doi.org/10.1016/j.nbd.2022.105946.
[5] Kuburas A, Russo AF. (2023). Shared and independent roles of CGRP and PACAP in migraine pathophysiology. J Headache Pain. 2023;24(1):34. https://doi.org/10.1186/s10194-023-01569-2.
[6] Jacobs B, Dussor G. (2016). Neurovascular contributions to migraine: Moving beyond vasodilation. Neuroscience. 2016;338:130-44. https://doi.org/10.1016/j.neuroscience.2016.06.012.
[7] Ray B, Wolff H. (1940). Experimental studies on headache. Pain sensitive structures of the head and their significance in headache. Arch Surg. 1940;41(4):813-56. https://doi.org/10.1001/archsurg.1940.01210040002001.
[8] Tunis MM, Wolff HG. (1953). Studies on headache; long-term observations of the reactivity of the cranial arteries in subjects with vascular headache of the migraine type. AMA Arch Neurol Psychiatry. 1953;70(5):551-7. https://doi.org/10.1001/archneurpsyc.1953.02320350003001.
[9] Goadsby PJ. (2009). The vascular theory of migraine—a great story wrecked by the facts. Brain. 2009;132(Pt 1):6-7. https://doi.org/10.1093/brain/awn321.
[10] Ashina M. (2020). Migraine. N Engl J Med. 2020;383(19):1866-76. https://doi.org/10.1056/NEJMra1915327.
[11] Rahmann A, Wienecke T, Hansen JM, Fahrenkrug J, Olesen J, Ashina M. (2008). Vasoactive intestinal peptide causes marked cephalic vasodilation, but does not induce migraine. Cephalalgia. 2008;28(3):226-36. https://doi.org/10.1111/j.1468-2982.2007.01497.x.
[12] Pellesi L, Al-Karagholi MA, De Icco R, Coskun H, Elbahi FA, Lopez-Lopez C, et al. (2021). Effect of Vasoactive Intestinal Polypeptide on Development of Migraine Headaches: A Randomized Clinical Trial. JAMA Netw Open. 2021;4(8):e2118543. https://doi.org/10.1001/jamanetworkopen.2021.18543.
[13] Ramachandran R. (2018). Neurogenic inflammation and its role in migraine. Semin Immunopathol. 2018;40(3):301-14. https://doi.org/10.1007/s00281-018-0676-y.
[14] Stankewitz A, Keidel L, Rehm M, Irving S, Kaczmarz S, Preibisch C, et al. (2021). Migraine attacks as a result of hypothalamic loss of control. Neuroimage Clin. 2021;32:102784. https://doi.org/10.1016/j.nicl.2021.102784.
[15] Gollion C, De Icco R, Dodick DW, Ashina H. (2022). The premonitory phase of migraine is due to hypothalamic dysfunction: revisiting the evidence. J Headache Pain. 2022;23(1):158. https://doi.org/10.1186/s10194-022-01518-5.
[16] Malu OO, Bailey J, Hawks MK. (2022). Cluster Headache: Rapid Evidence Review. Am Fam Physician. 2022;105(1):24-32.
[17] Steel SJ, Robertson CE, Whealy MA. (2021). Current Understanding of the Pathophysiology and Approach to Tension-Type Headache. Curr Neurol Neurosci Rep. 2021;21(10):56. https://doi.org/10.1007/s11910-021-01138-7.
[18] Edvinsson L, Goadsby PJ. (2019). Discovery of CGRP in relation to migraine. Cephalalgia. 2019;39(3):331-2. https://doi.org/10.1177/0333102418779544.
[19] Bedrin K, Shah T, Vaidya S, Ailani J. (2024). CGRP Modulating Therapies: An Update. Curr Neurol Neurosci Rep. 2024;24(9):453-9. https://doi.org/10.1007/s11910-024-01363-w.
[20] Gárate G, Pascual J, Pascual-Mato M, Madera J, Martín MM, González-Quintanilla V. (2024). Untangling the mess of CGRP levels as a migraine biomarker: an in-depth literature review and analysis of our experimental experience. J Headache Pain. 2024;25(1):69. https://doi.org/10.1186/s10194-024-01769-4.
[21] Kamm K. (2022). CGRP and Migraine: What Have We Learned From Measuring CGRP in Migraine Patients So Far? Front Neurol. 2022;13:930383. https://doi.org/10.3389/fneur.2022.930383.
[22] Kamm K, Straube A, Ruscheweyh R. (2019). Calcitonin gene-related peptide levels in tear fluid are elevated in migraine patients compared to healthy controls. Cephalalgia. 2019;39(12):1535-43. https://doi.org/10.1177/0333102419856640.
[23] Alpuente A, Gallardo VJ, Asskour L, Caronna E, Torres-Ferrus M, Pozo-Rosich P. (2022). Salivary CGRP can monitor the different migraine phases: CGRP (in)dependent attacks. Cephalalgia. 2022;42(3):186-96. https://doi.org/10.1177/03331024211040467.
[24] Waliszewska-Prosół M, Vuralli D, Martelletti P. (2023). What to do with non-responders to CGRP(r) monoclonal antibodies: switch to another or move to gepants? J Headache Pain. 2023;24(1):163. https://doi.org/10.1186/s10194-023-01698-8.
[25] An YC, Hung KS, Liang CS, Tsai CK, Tsai CL, Chen SJ, et al. (2024). Genetic variants associated with response to anti-CGRP monoclonal antibody therapy in a chronic migraine Han Chinese population. J Headache Pain. 2024;25(1):149. https://doi.org/10.1186/s10194-024-01850-y.
[26] Pellesi L, Ashina M, Martelletti P. (2024). Targeting the PACAP-38 pathway is an emerging therapeutic strategy for migraine prevention. Expert Opin Emerg Drugs. 2024;29(1):57-64. https://doi.org/10.1080/14728214.2024.2317778.
[27] Pellesi L, De Icco R, Al-Karagholi MA, Ashina M. (2020). Reducing Episodic Cluster Headaches: Focus on Galcanezumab. J Pain Res. 2020;13:1591-9. https://doi.org/10.2147/JPR.S222604.
[28] Medrea I, Christie S, Tepper SJ, Thavorn K, Hutton B. (2022). Effects of acute and preventive therapies for episodic and chronic cluster headache: A scoping review of the literature. Headache. 2022;62(3):329-62. https://doi.org/10.1111/head.14284.
[29] Petersen AS, Lund N, Goadsby PJ, Belin AC, Wang SJ, Fronczek R, et al. (2024). Recent advances in diagnosing, managing, and understanding the pathophysiology of cluster headache. Lancet Neurol. 2024;23(7):712-24. https://doi.org/10.1016/S1474-4422(24)00143-1.
[30] Gupta R, Ahmed T, Banerjee B, Bhatia M. (2009). Plasma calcitonin gene-related peptide concentration is comparable to control group among migraineurs and tension type headache subjects during inter-ictal period. J Headache Pain. 2009;10(3):161-6. https://doi.org/10.1007/s10194-009-0110-x.
[31] Bach FW, Langemark M, Ekman R, Rehfeld JF, Schifter S, Olesen J. (1994). Effect of sulpiride or paroxetine on cerebrospinal fluid neuropeptide concentrations in patients with chronic tension-type headache. Neuropeptides. 1994;27(2):129-36. https://doi.org/10.1016/0143-4179(94)90053-1.
[32] Moller K, Zhang YZ, Håkanson R, Luts A, Sjölund B, Uddman R, et al. (1993). Pituitary adenylate cyclase activating peptide is a sensory neuropeptide: immunocytochemical and immunochemical evidence. Neuroscience. 1993;57(3):725-32. https://doi.org/10.1016/0306-4522(93)90018-b.
[33] Mulder H, Uddman R, Moller K, Zhang YZ, Ekblad E, Alumets J, et al. (1994). Pituitary adenylate cyclase activating polypeptide expression in sensory neurons. Neuroscience. 1994;63(1):307-12. https://doi.org/10.1016/0306-4522(94)90025-6.
[34] Edvinsson L, Elsås T, Suzuki N, Shimizu T, Lee TJ. (2001). Origin and co-localization of nitric oxide synthase, CGRP, PACAP, and VIP in the cerebral circulation of the rat. Microsc Res Tech. 2001;53(3):221-8. https://doi.org/10.1002/jemt.1086.
[35] Ashina M, Phul R, Khodaie M, Löf E, Florea I. (2024). A Monoclonal Antibody to PACAP for Migraine Prevention. N Engl J Med. 2024;391(9):800-9. https://doi.org/10.1056/NEJMoa2314577.
[36] Ashina M, Doležil D, Bonner JH, Zhou L, Klatt J, Picard H, et al. (2021). A phase 2, randomized, double-blind, placebo-controlled trial of AMG 301, a pituitary adenylate cyclase-activating polypeptide PAC1 receptor monoclonal antibody for migraine prevention. Cephalalgia. 2021;41(1):33-44. https://doi.org/10.1177/0333102420970889.
[37] Guo S, Rasmussen RH, Hay-Schmidt A, Ashina M, Asuni AA, Jensen JM, et al. (2024). VPAC1 and VPAC2 receptors mediate tactile hindpaw hypersensitivity and carotid artery dilatation induced by PACAP38 in a migraine relevant mouse model. J Headache Pain. 2024;25(1):126. https://doi.org/10.1186/s10194-024-01830-2.
[38] Pedersen SH, la Cour SH, Calloe K, Hauser F, Olesen J, Klaerke DA, et al. (2019). PACAP-38 and PACAP(6-38) Degranulate Rat Meningeal Mast Cells via the Orphan MrgB3-Receptor. Front Cell Neurosci. 2019;13:114. https://doi.org/10.3389/fncel.2019.00114.
[39] Staton PC, Hatcher JP, Walker DJ, Morrison AD, Shapland EM, Hughes JP, et al. (2008). The putative cannabinoid receptor GPR55 plays a role in mechanical hyperalgesia associated with inflammatory and neuropathic pain. Pain. 2008;139(1):225-36. https://doi.org/10.1016/j.pain.2008.04.006.
[40] Han X, Dong Z, Hou L, Wan D, Chen M, Tang W, et al. (2015). Interictal plasma pituitary adenylate cyclase-activating polypeptide levels are decreased in migraineurs but remain unchanged in patients with tension-type headache. Clin Chim Acta. 2015;450:151-4. https://doi.org/10.1016/j.cca.2015.08.017.
[41] Tuka B, Szabó N, Tóth E, Kincses ZT, Párdutz Á, Szok D, et al. (2016). Release of PACAP-38 in episodic cluster headache patients—an exploratory study. J Headache Pain. 2016;17(1):69. https://doi.org/10.1186/s10194-016-0660-7.
[42] Vollesen ALH, Snoer A, Chaudhry B, Petersen AS, Hagedorn A, Hoffmann J, et al. (2020). The effect of pituitary adenylate cyclase-activating peptide-38 and vasoactive intestinal peptide in cluster headache. Cephalalgia. 2020;40(13):1474-88. https://doi.org/10.1177/0333102420940689.
[43] Pellesi L, Chaudhry BA, Vollesen ALH, Snoer AH, Baumann K, Skov PS, et al. (2022). PACAP38- and VIP-induced cluster headache attacks are not associated with changes of plasma CGRP or markers of mast cell activation. Cephalalgia. 2022;42(8):687-95. https://doi.org/10.1177/03331024211056248.
[44] Deligianni C, Pellesi L, Chaudhry BA, Haulund Vollesen AL, Snoer AH, Hannibal J, et al. (2023). Plasma levels of VIP are not elevated during PACAP- and VIP-induced cluster headache attacks: an exploratory study. Front Neurol. 2023;14:1135246. https://doi.org/10.3389/fneur.2023.1135246.
[45] Tanaka M, Szabó Á, Körtési T, Szok D, Tajti J, Vécsei L. (2023). From CGRP to PACAP, VIP, and Beyond: Unraveling the Next Chapters in Migraine Treatment. Cells. 2023;12(22):2649. https://doi.org/10.3390/cells12222649.
Type
Published
Data Availability Statement
Not applicable.
Issue
Section
License
Copyright (c) 2025 Brain Conflux

This work is licensed under a Creative Commons Attribution 4.0 International License.







