Trends and Cross-Country Inequalities of Melanoma andNon-Melanoma Skin Cancer from 1990 to 2021 and Predictive Trendsfrom 2022 to 2044: A Global Burden of Disease Study
DOI:
https://doi.org/10.71321/pykzbr95Keywords:
Trend, Inequality, Global burden of disease, Melanoma, Non-melanoma skin cancerAbstract
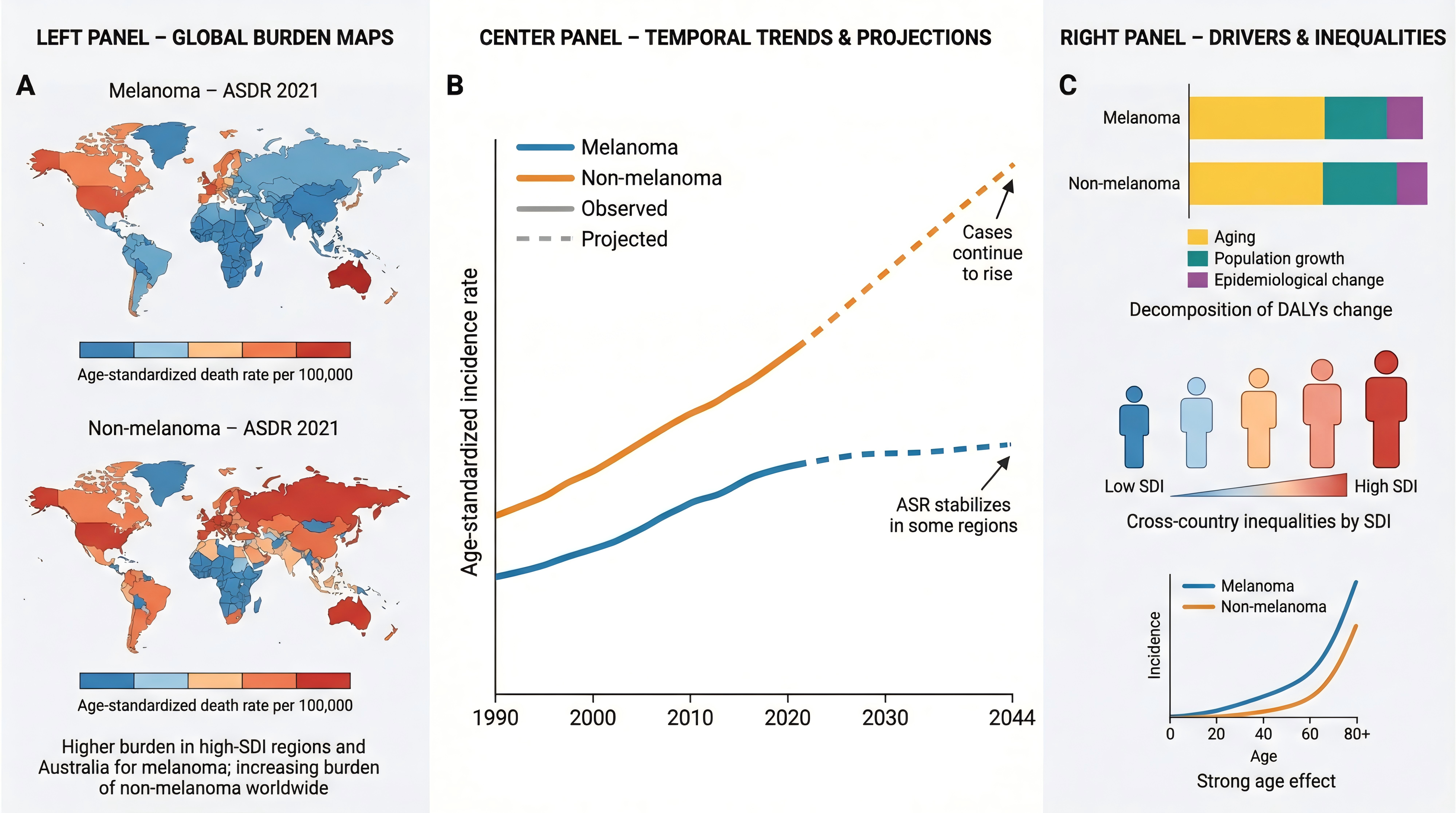
Background: Malignant skin melanoma (MSM) and non-melanoma skin cancer (NMSC) have imposed a significant health and economic burden globally. This study aims to explore the disease burden and temporal trends of MSM and NMSC to inform evidence-based prevention and control strategies.
Methods: Data were derived from the Global Burden of Diseases (GBD) database, covering deaths, disability-adjusted life years (DALYs), incidence, and prevalence. Joinpoint regression, inequality analysis, decomposition analysis and age-period-cohort analysis identified trends and revealed the causes of burden changes from 1990 to 2021. Nordpred package in R projected the future trends of MSM and NMSC from 2022 to 2044.
Results: From 1990 to 2021, global trends showed an increase in the number of deaths, DALYs, incidence, and prevalence for MSM, squamous cell carcinoma (SCC), and basal cell carcinoma (BCC). The disease burden was highest in high Socio-Demographic Index (SDI) regions, predominantly concentrated in New Zealand, Australia, and the United States. Among MSM, SCC and BCC, SCC experienced the most substantial increases in age-standardized incidence (AAPC = 1.62 [95% CI: 1.51 to 1.73]) and prevalence (AAPC = 1.90 [95% CI: 1.78 to 2.02]). The primary drivers of changes in DALYs were identified as population aging and population growth. Persistent health inequalities continue to exist in the global burden of skin cancer. In the future, the deaths, DALYs, incidence, and prevalence cases of MSM and NMSC may continue to increase.
Conclusion: The disease burden associated with MSM and NMSC remains substantial. Primary prevention for the elderly should be given priority. In the prevention of skin cancer, particular attention should be directed toward SCC. Global medical resources should be appropriately tilted towards skin cancer.
References
[1] Villani A, Potestio L, Fabbrocini G, Scalvenzi M. (2022). New Emerging Treatment Options for Advanced Basal Cell Carcinoma and Squamous Cell Carcinoma. Adv Ther, 39(3), 1164-1178. https://doi.org/10.1007/s12325-022-02044-1
[2] D'Mello SA, Finlay GJ, Baguley BC, Askarian-Amiri ME. (2016). Signaling Pathways in Melanogenesis. Int J Mol Sci, 17(7). https://doi.org/10.3390/ijms17071144
[3] Fania L, Didona D, Di Pietro FR, Verkhovskaia S, Morese R, Paolino G, et al. (2021). Cutaneous Squamous Cell Carcinoma: From Pathophysiology to Novel Therapeutic Approaches. Biomedicines, 9(2). https://doi.org/10.3390/biomedicines9020171
[4] Chen OM, Kim K, Steele C, Wilmas KM, Aboul-Fettouh N, Burns C, et al. (2022). Advances in Management and Therapeutics of Cutaneous Basal Cell Carcinoma. Cancers (Basel), 14(15). https://doi.org/10.3390/cancers14153720
[5] Radiotis G, Roberts N, Czajkowska Z, Khanna M, Körner A. (2014). Nonmelanoma skin cancer: disease-specific quality-of-life concerns and distress. Oncol Nurs Forum, 41(1), 57-65. https://doi.org/10.1188/14.Onf.57-65
[6] Sahu S, Yosipovitch G. (2021). Itch and pain intensity in skin cancer: Why should dermatologic surgeons assess it? Clin Dermatol, 39(1), 119-122. https://doi.org/10.1016/j.clindermatol.2020.05.001
[7] Venger O, Zhulkevych I, & Mysula Y. (2021). PSYCHOLOGICAL AND PSYCHOPATHOLOGICAL FEATURES OF PATIENTS WITH SKIN CANCER. Georgian Med News, (315), 29-33.
[8] Sabit H, Kaliyadan F, Menezes RG. (2020). Malignant melanoma: Underlying epigenetic mechanisms. Indian J Dermatol Venereol Leprol, 86(5), 475-481. https://doi.org/10.4103/ijdvl.IJDVL_791_19
[9] Schadendorf D, van Akkooi ACJ, Berking C, Griewank KG, Gutzmer R, Hauschild A, et al. (2018). Melanoma. Lancet, 392(10151), 971-984. https://doi.org/10.1016/s0140-6736(18)31559-9
[10] Yusuf N. (2023). Immunomodulation of Skin Cancer. Int J Mol Sci, 24(13). https://doi.org/10.3390/ijms241310462
[11] Gordon LG, Rowell D. (2015). Health system costs of skin cancer and cost-effectiveness of skin cancer prevention and screening: a systematic review. Eur J Cancer Prev, 24(2), 141-149. https://doi.org/10.1097/cej.0000000000000056
[12] Kao SZ, Ekwueme DU, Holman DM, Rim SH, Thomas CC, & Saraiya M. (2023). Economic burden of skin cancer treatment in the USA: an analysis of the Medical Expenditure Panel Survey Data, 2012-2018. Cancer Causes Control, 34(3), 205-212. https://doi.org/10.1007/s10552-022-01644-0
[13] Akdeniz M, Hahnel E, Ulrich C, Blume-Peytavi U, & Kottner J. (2019). Prevalence and associated factors of skin cancer in aged nursing home residents: A multicenter prevalence study. PLoS One, 14(4), e0215379. https://doi.org/10.1371/journal.pone.0215379
[14] Aggarwal P, Knabel P, & Fleischer AB, Jr. (2021). United States burden of melanoma and non-melanoma skin cancer from 1990 to 2019. J Am Acad Dermatol, 85(2), 388-395. https://doi.org/10.1016/j.jaad.2021.03.109
[15] Wang M, Gao X, & Zhang L. (2024). Recent global patterns in skin cancer incidence, mortality, and prevalence. Chin Med J (Engl), 10.1097/cm9.0000000000003416. https://doi.org/10.1097/cm9.0000000000003416
[16] Zhang W, Zeng W, Jiang A, He Z, Shen X, Dong X, et al. (2021). Global, regional and national incidence, mortality and disability-adjusted life-years of skin cancers and trend analysis from 1990 to 2019: An analysis of the Global Burden of Disease Study 2019. Cancer Med, 10(14), 4905-4922. https://doi.org/10.1002/cam4.4046
[17] Zhou L, Zhong Y, Han L, Xie Y, & Wan M. (2025). Global, regional, and national trends in the burden of melanoma and non-melanoma skin cancer: insights from the global burden of disease study 1990-2021. Sci Rep, 15(1), 5996. https://doi.org/10.1038/s41598-025-90485-3
[18] Wang R, Chen Y, Shao X, Chen T, Zhong J, Ou Y, et al. (2025). Burden of Skin Cancer in Older Adults From 1990 to 2021 and Modelled Projection to 2050. JAMA Dermatol, 10.1001/jamadermatol.2025.1276. https://doi.org/10.1001/jamadermatol.2025.1276
[19] Yu G, Gong X, Xu Y, Sun H, Liu Y, Zhai C, et al. (2023). The global burden and trends of four major types of heart disease, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Public Health, 220, 1-9. https://doi.org/10.1016/j.puhe.2023.04.005
[20] Wang F, Hu D, Sun H, Yan Z, Wang Y, Wang L, et al. (2023). Global, regional, and national burden of digestive diseases: findings from the global burden of disease study 2019. Front Public Health, 11, 1202980. https://doi.org/10.3389/fpubh.2023.1202980
[21] Wyper GMA, Grant I, Fletcher E, McCartney G, Fischbacher C, & Stockton DL. (2020). How do world and European standard populations impact burden of disease studies? A case study of disability-adjusted life years (DALYs) in Scotland. Arch Public Health, 78, 1. https://doi.org/10.1186/s13690-019-0383-8
[22] Kim HJ, Fay MP, Feuer EJ, & Midthune DN. (2000). Permutation tests for joinpoint regression with applications to cancer rates. Stat Med, 19(3), 335-351. https://doi.org/10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z
[23] Chen Q, Li T, Ding H, Huang G, Du D, & Yang J. (2024). Age-period-cohort analysis of epidemiological trends in pelvic fracture in China from 1992 to 2021 and forecasts for 2046. Front Public Health, 12, 1428068. https://doi.org/10.3389/fpubh.2024.1428068
[24] Su Z, Zou Z, Hay SI, Liu Y, Li S, Chen H, et al. (2022). Global, regional, and national time trends in mortality for congenital heart disease, 1990-2019: An age-period-cohort analysis for the Global Burden of Disease 2019 study. EClinicalMedicine, 43, 101249. https://doi.org/10.1016/j.eclinm.2021.101249
[25] Liu C, Zhu S, Zhang J, Wu P, Wang X, Du S, et al. (2023). Global, regional, and national burden of liver cancer due to non-alcoholic steatohepatitis, 1990-2019: a decomposition and age-period-cohort analysis. J Gastroenterol, 58(12), 1222-1236. https://doi.org/10.1007/s00535-023-02040-4
[26] Xie Y, Bowe B, Mokdad AH, Xian H, Yan Y, Li T, et al. (2018). Analysis of the Global Burden of Disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int, 94(3), 567-581. https://doi.org/10.1016/j.kint.2018.04.011
[27] Barboza-Solis C, Herrero R, & Fantin R. (2024). Health inequalities in a middle-income country: a systematic review of the Costa Rican case. Front Public Health, 12, 1397576. https://doi.org/10.3389/fpubh.2024.1397576
[28] Huang L, & He J. (2024). Trend analysis of hematological tumors in adolescents and young adults from 1990 to 2019 and predictive trends from 2020 to 2044: A Global Burden of Disease study. Cancer Med, 13(18), e70224. https://doi.org/10.1002/cam4.70224
[29] Valery PC, Laversanne M, Clark PJ, Petrick JL, McGlynn KA, & Bray F. (2018). Projections of primary liver cancer to 2030 in 30 countries worldwide. Hepatology, 67(2), 600-611. https://doi.org/10.1002/hep.29498
[30] D'Ambrosio AE, Albonico G, Enide I, Mordà O, Maisano M, & Mondello B. (2021). Pleural Melanoma Metastasis. Ann Thorac Surg, 112(2), e103-e105. https://doi.org/10.1016/j.athoracsur.2020.09.088
[31] Nakagawa T, Cho J, & Yeung DY. (2021). Successful Aging in East Asia: Comparison Among China, Korea, and Japan. J Gerontol B Psychol Sci Soc Sci, 76(Suppl 1), S17-s26. https://doi.org/10.1093/geronb/gbaa042
[32] Abbas K, Qadir MI, & Anwar S. (2019). The Role of Melanin in Skin Cancer. Crit Rev Eukaryot Gene Expr, 29(1), 17-24. https://doi.org/10.1615/CritRevEukaryotGeneExpr.2018024980
[33] Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. (2022). Lancet Psychiatry, 9(2), 137-150. https://doi.org/10.1016/s2215-0366(21)00395-3
[34] Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. (2022). Lancet Public Health, 7(2), e105-e125. https://doi.org/10.1016/s2468-2667(21)00249-8
[35] Huang J, Chan SC, Ko S, Lok V, Zhang L, Lin X, et al. (2023). Global Incidence, Mortality, Risk Factors and Trends of Melanoma: A Systematic Analysis of Registries. Am J Clin Dermatol, 24(6), 965-975. https://doi.org/10.1007/s40257-023-00795-3
[36] Liu-Smith F, Farhat AM, Arce A, Ziogas A, Taylor T, Wang Z, et al. (2017). Sex differences in the association of cutaneous melanoma incidence rates and geographic ultraviolet light exposure. J Am Acad Dermatol, 76(3), 499-505.e493. https://doi.org/10.1016/j.jaad.2016.08.027
[37] Modenese A, Korpinen L, & Gobba F. (2018). Solar Radiation Exposure and Outdoor Work: An Underestimated Occupational Risk. Int J Environ Res Public Health, 15(10). https://doi.org/10.3390/ijerph15102063
[38] Adams GJ, Goldstein EK, Goldstein BG, Jarman KL, & Goldstein AO. (2021). Attitudes and Behaviors That Impact Skin Cancer Risk among Men. Int J Environ Res Public Health, 18(19). https://doi.org/10.3390/ijerph18199989
[39] Kato J, Horimoto K, Sato S, Minowa T, & Uhara H. (2019). Dermoscopy of Melanoma and Non-melanoma Skin Cancers. Front Med (Lausanne), 6, 180. https://doi.org/10.3389/fmed.2019.00180
[40] Khayyati Kohnehshahri M, Sarkesh A, Mohamed Khosroshahi L, HajiEsmailPoor Z, Aghebati-Maleki A, Yousefi M, et al. (2023). Current status of skin cancers with a focus on immunology and immunotherapy. Cancer Cell Int, 23(1), 174. https://doi.org/10.1186/s12935-023-03012-7
[41] Alonso-Belmonte C, Montero-Vilchez T, Arias-Santiago S, & Buendía-Eisman A. (2022). Current State of Skin Cancer Prevention: A Systematic Review. Actas Dermosifiliogr, 113(8), 781-791. https://doi.org/10.1016/j.ad.2022.04.015 (Situación actual de la prevención del cáncer de piel: una revisión sistemática.)
[42] Saginala K, Barsouk A, Aluru JS, Rawla P, & Barsouk A. (2021). Epidemiology of Melanoma. Med Sci (Basel), 9(4). https://doi.org/10.3390/medsci9040063
[43] Farage MA, Miller KW, Berardesca E, & Maibach HI. (2009). Clinical implications of aging skin: cutaneous disorders in the elderly. Am J Clin Dermatol, 10(2), 73-86. https://doi.org/10.2165/00128071-200910020-00001
[44] Moriwaki S, & Takahashi Y. (2008). Photoaging and DNA repair. J Dermatol Sci, 50(3), 169-176. https://doi.org/10.1016/j.jdermsci.2007.08.011
[45] Wang S, Dong Z, & Wan X. (2024). Global, regional, and national burden of inflammatory bowel disease and its associated anemia, 1990 to 2019 and predictions to 2050: An analysis of the global burden of disease study 2019. Autoimmun Rev, 23(3), 103498. https://doi.org/10.1016/j.autrev.2023.103498
[46] Zhang H, Xue R, Kong X, Zhao M, & Jin Z. (2025). Global, regional, and national burden and projections to 2050 of occupational carcinogen-attributable nasopharyngeal and laryngeal cancer: a comprehensive analysis from the GBD 2021 study. Front Public Health, 13, 1615378. https://doi.org/10.3389/fpubh.2025.1615378
[47] Li Q, Xiao N, Zhang H, Liang G, Lin Y, Qian Z, et al. (2025). Systemic aging and aging-related diseases. Faseb j, 39(5), e70430. https://doi.org/10.1096/fj.202402479RRR
Type
Published
Data Availability Statement
All data used in this research are publicly available at http://ghdx.healthdata.org/gbd-results-tool.
Issue
Section
License
Copyright (c) 2026 Life Conflux

This work is licensed under a Creative Commons Attribution 4.0 International License.







