Tinnitus and Risk of Mortality in Normal-Hearing U.S. Adults: A Weighted Study Adjusted for Covariate Balance
DOI:
https://doi.org/10.71321/2eyyzr69Keywords:
tinnitus, mortality, balance, normal hearing, National Health and Nutrition Examination Survey (NHANES)Abstract
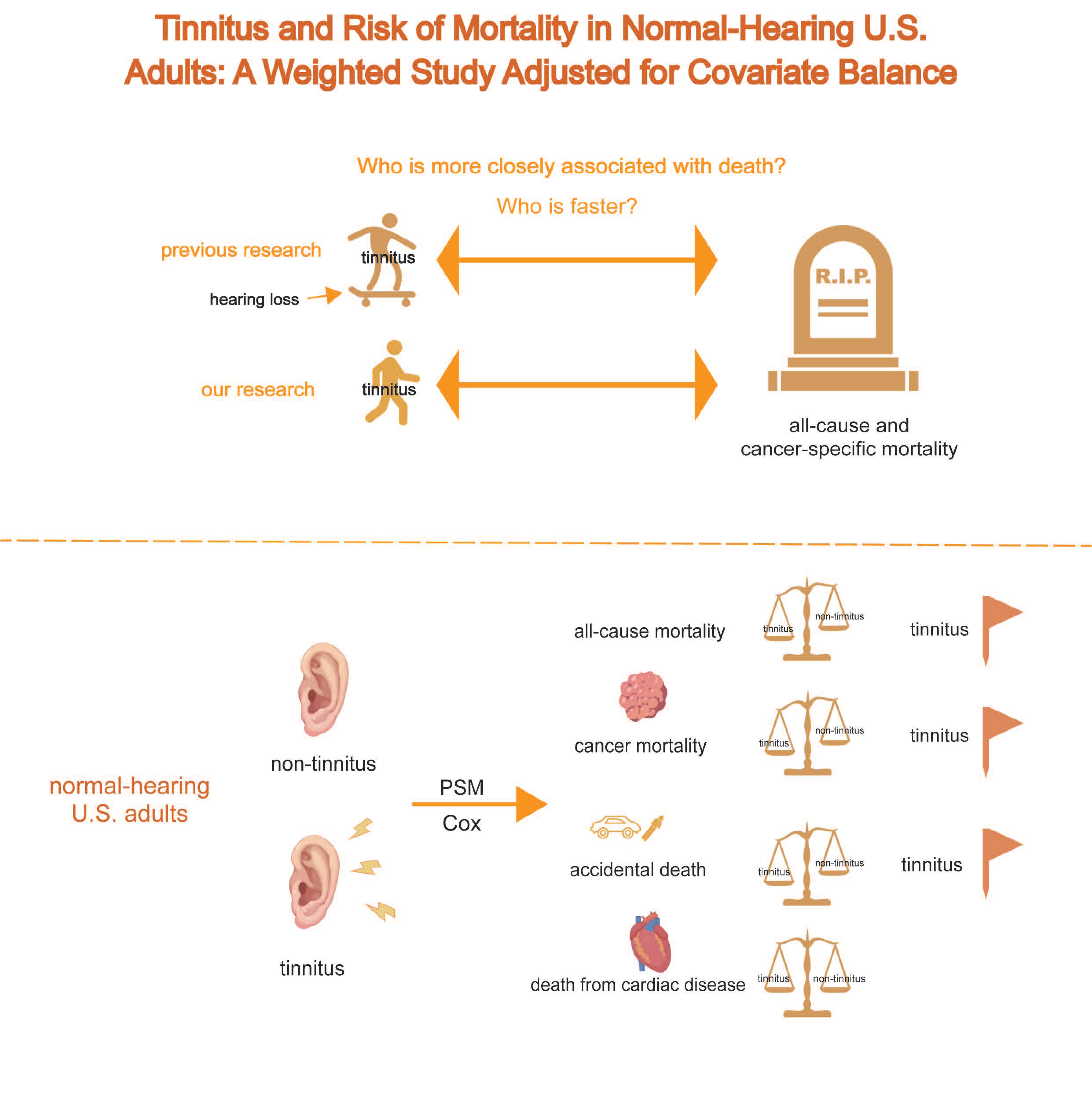
Background: Tinnitus and hearing loss are both prevalent chronic conditions that can significantly impair quality of life. While prior studies have explored the association between tinnitus and mortality, many have failed to isolate the effect of tinnitus from that of coexisting hearing loss—a frequent comorbidity—which may have introduced confounding and biased the results. To investigate the association between tinnitus and both all-cause and cause-specific mortality among U.S. adults aged 20-69 years with normal hearing.
Methods: We conducted a population-based cross-sectional analysis using data from five cycles of the National Health and Nutrition Examination Survey. Adults aged 20-69 years with audiometrically confirmed normal hearing were included. Tinnitus status was self-reported. Key covariates included demographic characteristics, comorbid conditions etc. We implemented propensity score matching and multivariable-adjusted Cox proportional hazards models to estimate the hazard ratios (HRs) for all-cause and cause-specific mortality.
Results: Tinnitus was found to be significantly associated with an increased risk of all-cause mortality (HR: 1.84; 95% CI: 1.38-2.44). A particularly elevated risk was observed for cancer-specific mortality (HR: 2.11; 95% CI: 1.26-3.58). Importantly, these findings persisted after adjusting for multiple covariates in the matched cohort, highlighting the robustness of the results derived from a balanced comparison.
Conclusions: Among U.S. adults with normal hearing, tinnitus was independently associated with increased risks of all-cause and cancer-specific mortality. These findings underscore the importance of recognizing tinnitus as not merely a benign symptom, but a potential marker of broader health risks, even in individuals without hearing impairment.
References
[1] Baguley D, McFerran D, Hall D. (2013) Tinnitus. Lancet (London, England).382(9904):1600-7 https://doi.org/10.1016/s0140-6736(13)60142-7.
[2] Langguth B, Kreuzer PM, Kleinjung T, De Ridder D. (2013) Tinnitus: causes and clinical management. The Lancet Neurology.12(9):920-30 https://doi.org/10.1016/s1474-4422(13)70160-1.
[3] Sharma A, Sood N, Munjal S, Panda N. (2021) Perception of Tinnitus Handicap And Stress Across Age Groups in Normal Hearing. The international tinnitus journal.25(1):13-7 https://doi.org/10.5935/0946-5448.2020004.
[4] Tunkel DE, Bauer CA, Sun GH, Rosenfeld RM, Chandrasekhar SS, Cunningham ER, Jr., et al. (2014) Clinical practice guideline: tinnitus. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery.151(2 Suppl):S1-s40 https://doi.org/10.1177/0194599814545325.
[5] Jafari Z, Kolb BE, Mohajerani MH. (2019) Age-related hearing loss and tinnitus, dementia risk, and auditory amplification outcomes. Ageing research reviews.56:100963 https://doi.org/10.1016/j.arr.2019.100963.
[6] Friberg E, Jansson C, Mittendorfer-Rutz E, Rosenhall U, Alexanderson K. (2012) Sickness absence due to otoaudiological diagnoses and risk of disability pension: a nationwide Swedish prospective cohort study. PloS one.7(1):e29966 https://doi.org/10.1371/journal.pone.0029966.
[7] Esmaili AA, Renton J. (2018) A review of tinnitus. Australian journal of general practice.47(4):205-8 https://doi.org/10.31128/ajgp-12-17-4420.
[8] Choi J, Lee CH, Kim SY. (2021) Association of Tinnitus with Depression in a Normal Hearing Population. Medicina (Kaunas, Lithuania).57(2) https://doi.org/10.3390/medicina57020114.
[9] Granjeiro RC, Kehrle HM, de Oliveira TS, Sampaio AL, de Oliveira CA. (2013) Is the degree of discomfort caused by tinnitus in normal-hearing individuals correlated with psychiatric disorders? Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery.148(4):658-63 https://doi.org/10.1177/0194599812473554.
[10] Huang YS, Koo M, Chen JC, Hwang JH. (2017) The association between tinnitus and the risk of ischemic cerebrovascular disease in young and middle-aged patients: A secondary case-control analysis of a nationwide, population-based health claims database. PloS one.12(11):e0187474 https://doi.org/10.1371/journal.pone.0187474.
[11] Chu HT, Liang CS, Yeh TC, Hu LY, Yang AC, Tsai SJ, et al. (2020) Tinnitus and risk of Alzheimer's and Parkinson's disease: a retrospective nationwide population-based cohort study. Scientific reports.10(1):12134 https://doi.org/10.1038/s41598-020-69243-0.
[12] Loiselle AR, Neustaeter A, de Kleine E, van Dijk P, Jansonius NM. (2020) Associations between tinnitus and glaucoma suggest a common mechanism: A clinical and population-based study. Hearing research.386:107862 https://doi.org/10.1016/j.heares.2019.107862.
[13] Hoare DJ, Edmondson-Jones M, Sereda M, Akeroyd MA, Hall D. (2014) Amplification with hearing aids for patients with tinnitus and co-existing hearing loss. The Cochrane database of systematic reviews(1):Cd010151 https://doi.org/10.1002/14651858.CD010151.pub2.
[14] Xiong B, Liu Z, Liu Q, Peng Y, Wu H, Lin Y, et al. (2019) Missed hearing loss in tinnitus patients with normal audiograms. Hearing research.384:107826 https://doi.org/10.1016/j.heares.2019.107826.
[15] Parthasarathy S, Shetty HN. (2021) Manipulation of Hearing Aid Gain and Tinnitus Relief: A Paired Comparison Study. The journal of international advanced otology.17(2):145-9 https://doi.org/10.5152/jiao.2021.8873.
[16] Yoo HB, De Ridder D, Vanneste S. (2016) White Matter Changes in Tinnitus: Is It All Age and Hearing Loss? Brain connectivity.6(1):84-93 https://doi.org/10.1089/brain.2015.0380.
[17] Matamala MF, Nogales FF, Lardelli P, Navarro N. (1987) Metastatic granulosa cell tumor with pattern of sex cord tumor with annular tubules. International journal of gynecological pathology : official journal of the International Society of Gynecological Pathologists.6(2):185-93 https://doi.org/10.1097/00004347-198706000-00010.
[18] Clifford RE, Maihofer AX, Chatzinakos C, Coleman JRI, Daskalakis NP, Gasperi M, et al. (2024) Genetic architecture distinguishes tinnitus from hearing loss. Nature communications.15(1):614 https://doi.org/10.1038/s41467-024-44842-x.
[19] Williams W, Carter L. (2017) Tinnitus and leisure noise. International journal of audiology.56(4):219-25 https://doi.org/10.1080/14992027.2016.1250961.
[20] Martines F, Sireci F, Cannizzaro E, Costanzo R, Martines E, Mucia M, et al. (2015) Clinical observations and risk factors for tinnitus in a Sicilian cohort. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery.272(10):2719-29 https://doi.org/10.1007/s00405-014-3275-0.
[21] Veile A, Zimmermann H, Lorenz E, Becher H. (2018) Is smoking a risk factor for tinnitus? A systematic review, meta-analysis and estimation of the population attributable risk in Germany. BMJ open.8(2):e016589 https://doi.org/10.1136/bmjopen-2017-016589.
[22] Arnold ML, Dhar S, Lee DJ, Perreira KM, Pupo D, Tsalatsanis A, et al. (2022) Sex-Specific Prevalence, Demographic Characteristics, and Risk Factors of Tinnitus in the Hispanic Community Health Study/Study of Latinos. American journal of audiology.31(1):78-90 https://doi.org/10.1044/2021_aja-21-00138.
[23] Mazurek B, Boecking B, Brueggemann P. (2019) Association Between Stress and Tinnitus-New Aspects. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology.40(4):e467-e73 https://doi.org/10.1097/mao.0000000000002180.
[24] Musleh A, Alshehri S, Qobty A. (2022) Hyperlipidemia and its relation with tinnitus: Cross-sectional approach. Nigerian journal of clinical practice.25(7):1046-9 https://doi.org/10.4103/njcp.njcp_1465_21.
[25] Boecking B, Klasing S, Walter M, Brueggemann P, Nyamaa A, Rose M, et al. (2022) Vascular-Metabolic Risk Factors and Psychological Stress in Patients with Chronic Tinnitus. Nutrients.14(11) https://doi.org/10.3390/nu14112256.
[26] Lin X, Liu Y, Chen Z, Wei Y, Lin J, Chen C, et al. (2023) Association between depression and tinnitus in US adults: A nationally representative sample. Laryngoscope investigative otolaryngology.8(5):1365-75 https://doi.org/10.1002/lio2.1134.
[27] Mahboubi H, Oliaei S, Kiumehr S, Dwabe S, Djalilian HR. (2013) The prevalence and characteristics of tinnitus in the youth population of the United States. The Laryngoscope.123(8):2001-8 https://doi.org/10.1002/lary.24015.
[28] Lin FR, Thorpe R, Gordon-Salant S, Ferrucci L. (2011) Hearing loss prevalence and risk factors among older adults in the United States. The journals of gerontology Series A, Biological sciences and medical sciences.66(5):582-90 https://doi.org/10.1093/gerona/glr002.
[29] Seo JH, Kang JM, Hwang SH, Han KD, Joo YH. (2016) Relationship between tinnitus and suicidal behaviour in Korean men and women: a cross-sectional study. Clinical otolaryngology : official journal of ENT-UK ; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery.41(3):222-7 https://doi.org/10.1111/coa.12500.
[30] Cheng YF, Xirasagar S, Kuo NW, Lin HC. (2023) Tinnitus and risk of attempted suicide: A one year follow-up study. Journal of affective disorders.322:141-5 https://doi.org/10.1016/j.jad.2022.11.009.
[31] Sanchez VA, Dinh PC, Jr., Rooker J, Monahan PO, Althouse SK, Fung C, et al. (2023) Prevalence and risk factors for ototoxicity after cisplatin-based chemotherapy. Journal of cancer survivorship : research and practice.17(1):27-39 https://doi.org/10.1007/s11764-022-01313-w.
[32] Feng X, Li W, Cheng M, Qiu W, Liang R, Li M, et al. (2022) Association of hearing loss with total and cause-specific mortality in US adults. Environmental science and pollution research international.29(4):5032-42 https://doi.org/10.1007/s11356-021-16038-z.
[33] Cao C, Cade WT, Li S, McMillan J, Friedenreich C, Yang L. (2021) Association of Balance Function With All-Cause and Cause-Specific Mortality Among US Adults. JAMA otolaryngology-- head & neck surgery.147(5):460-8 https://doi.org/10.1001/jamaoto.2021.0057.
[34] Martz E, Jelleberg C, Dougherty DD, Wolters C, Schneiderman A. (2018) Tinnitus, Depression, Anxiety, and Suicide in Recent Veterans: A Retrospective Analysis. Ear and hearing.39(6):1046-56 https://doi.org/10.1097/aud.0000000000000573.
[35] Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, et al. (2017) An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public health.152:157-71 https://doi.org/10.1016/j.puhe.2017.07.035.
[36] Miaskowski C, Mastick J, Paul SM, Abrams G, Cheung S, Sabes JH, et al. (2018) Impact of chemotherapy-induced neurotoxicities on adult cancer survivors' symptom burden and quality of life. Journal of cancer survivorship : research and practice.12(2):234-45 https://doi.org/10.1007/s11764-017-0662-8.
[37] Khan A, Mubdi N, Budnick A, Feldman DR, Williams SW, Patel S, et al. (2020) The experience of hearing loss in adult survivors of childhood and young adult cancer: A qualitative study. Cancer.126(8):1776-83 https://doi.org/10.1002/cncr.32698.
[38] Hébert S, Lupien SJ. (2007) The sound of stress: blunted cortisol reactivity to psychosocial stress in tinnitus sufferers. Neuroscience letters.411(2):138-42 https://doi.org/10.1016/j.neulet.2006.10.028.
[39] Hébert S, Lupien SJ. (2009) Salivary cortisol levels, subjective stress, and tinnitus intensity in tinnitus sufferers during noise exposure in the laboratory. International journal of hygiene and environmental health.212(1):37-44 https://doi.org/10.1016/j.ijheh.2007.11.005.
[40] Hébert S, Paiement P, Lupien SJ. (2004) A physiological correlate for the intolerance to both internal and external sounds. Hearing research.190(1-2):1-9 https://doi.org/10.1016/s0378-5955(04)00021-8.
[41] Hasson D, Theorell T, Liljeholm-Johansson Y, Canlon B. (2009) Psychosocial and physiological correlates of self-reported hearing problems in male and female musicians in symphony orchestras. International journal of psychophysiology : official journal of the International Organization of Psychophysiology.74(2):93-100 https://doi.org/10.1016/j.ijpsycho.2009.07.009.
[42] Friberg E, Rosenhall U, Alexanderson K. (2014) Sickness absence and disability pension due to otoaudiological diagnoses: risk of premature death--a nationwide prospective cohort study. BMC public health.14:137 https://doi.org/10.1186/1471-2458-14-137.
[43] Li YL, Hsu YC, Lin CY, Wu JL. (2022) Sleep disturbance and psychological distress in adult patients with tinnitus. Journal of the Formosan Medical Association = Taiwan yi zhi.121(5):995-1002 https://doi.org/10.1016/j.jfma.2021.07.022.
[44] Pearson SE, Taylor J, Hoare DJ, Patel P, Baguley DM. (2019) Exploring the Experiences of Cancer Patients With Chemotherapy-Induced Ototoxicity: Qualitative Study Using Online Health Care Forums. JMIR cancer.5(1):e10883 https://doi.org/10.2196/10883.
[45] Karaaslan Ö, Kantekin Y, Hacımusalar Y, Dağıstan H. (2020) Anxiety sensitivities, anxiety and depression levels, and personality traits of patients with chronic subjective tinnitus: a case-control study. International journal of psychiatry in clinical practice.24(3):264-9 https://doi.org/10.1080/13651501.2020.1757117.
[46] Hamer M, Chida Y, Molloy GJ. (2009) Psychological distress and cancer mortality. Journal of psychosomatic research.66(3):255-8 https://doi.org/10.1016/j.jpsychores.2008.11.002.
[47] Knight KR, Kraemer DF, Neuwelt EA. (2005) Ototoxicity in children receiving platinum chemotherapy: underestimating a commonly occurring toxicity that may influence academic and social development. Journal of clinical oncology : official journal of the American Society of Clinical Oncology.23(34):8588-96 https://doi.org/10.1200/jco.2004.00.5355.
[48] Bisht M, Bist SS. (2011) Ototoxicity: the hidden menace. Indian journal of otolaryngology and head and neck surgery : official publication of the Association of Otolaryngologists of India.63(3):255-9 https://doi.org/10.1007/s12070-011-0151-8.
[49] Diaz KM, Shimbo D. (2013) Physical activity and the prevention of hypertension. Current hypertension reports.15(6):659-68 https://doi.org/10.1007/s11906-013-0386-8.
[50] Ekelund U, Tarp J, Steene-Johannessen J, Hansen BH, Jefferis B, Fagerland MW, et al. (2019) Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: systematic review and harmonised meta-analysis. BMJ (Clinical research ed).366:l4570 https://doi.org/10.1136/bmj.l4570.
[51] Wade KH, Carslake D, Sattar N, Davey Smith G, Timpson NJ. (2018) BMI and Mortality in UK Biobank: Revised Estimates Using Mendelian Randomization. Obesity (Silver Spring, Md).26(11):1796-806 https://doi.org/10.1002/oby.22313.
[52] Özbey-Yücel Ü, Uçar A, Aydoğan Z, Tokgoz-Yilmaz S, Beton S. (2023) The effects of dietary and physical activity interventions on tinnitus symptoms: An RCT. Auris, nasus, larynx.50(1):40-7 https://doi.org/10.1016/j.anl.2022.04.013.
[53] Biswas R, Lugo A, Genitsaridi E, Trpchevska N, Akeroyd MA, Cederroth CR, et al. (2021) Modifiable lifestyle-related risk factors for tinnitus in the general population: An overview of smoking, alcohol, body mass index and caffeine intake. Progress in brain research.263:1-24 https://doi.org/10.1016/bs.pbr.2021.04.005.
[54] Feldman RD, Gros R. (2010) Rapid vascular effects of steroids - a question of balance? The Canadian journal of cardiology.26 Suppl A:22a-6a https://doi.org/10.1016/s0828-282x(10)71057-6.
[55] Berkel C, Cacan E. (2021) Estrogen- and estrogen receptor (ER)-mediated cisplatin chemoresistance in cancer. Life sciences.286:120029 https://doi.org/10.1016/j.lfs.2021.120029.
[56] Rajoria S, Hanly E, Nicolini A, George AL, Geliebter J, Shin EJ, et al. (2014) Interlinking of hypoxia and estrogen in thyroid cancer progression. Current medicinal chemistry.21(11):1351-60 https://doi.org/10.2174/0929867321666131201142434.
[57] Bruce DG, Devine A, Prince RL. (2002) Recreational physical activity levels in healthy older women: the importance of fear of falling. Journal of the American Geriatrics Society.50(1):84-9 https://doi.org/10.1046/j.1532-5415.2002.50012.x.
[58] Jefferis BJ, Iliffe S, Kendrick D, Kerse N, Trost S, Lennon LT, et al. (2014) How are falls and fear of falling associated with objectively measured physical activity in a cohort of community-dwelling older men? BMC geriatrics.14:114 https://doi.org/10.1186/1471-2318-14-114.
[59] Yang L, Cao C, Kantor ED, Nguyen LH, Zheng X, Park Y, et al. (2019) Trends in Sedentary Behavior Among the US Population, 2001-2016. Jama.321(16):1587-97 https://doi.org/10.1001/jama.2019.3636.
[60] Agrawal Y, Carey JP, Della Santina CC, Schubert MC, Minor LB. (2009) Disorders of balance and vestibular function in US adults: data from the National Health and Nutrition Examination Survey, 2001-2004. Archives of internal medicine.169(10):938-44 https://doi.org/10.1001/archinternmed.2009.66.
[61] McCarthy E, Marchese VG, Shipper AG, Rock K, Felter C. (2024) Identifying causes of balance impairment and exploring sensory contributions to balance in pediatric oncology: A scoping review. Critical reviews in oncology/hematology.201:104425 https://doi.org/10.1016/j.critrevonc.2024.104425.
[62] Mulvaney J, Dabdoub A. (2012) Atoh1, an essential transcription factor in neurogenesis and intestinal and inner ear development: function, regulation, and context dependency. Journal of the Association for Research in Otolaryngology : JARO.13(3):281-93 https://doi.org/10.1007/s10162-012-0317-4.
[63] Pearson SE, Caimino C, Shabbir M, Baguley DM. (2022) The impact of chemotherapy-induced inner ear damage on quality of life in cancer survivors: a qualitative study. Journal of cancer survivorship : research and practice.16(5):976-87 https://doi.org/10.1007/s11764-021-01089-5.
Type
Published
Data Availability Statement
The authors have no relevant financial or non-financial interests to disclose.
Issue
Section
License
Copyright (c) 2025 Life Conflux

This work is licensed under a Creative Commons Attribution 4.0 International License.







