Abnormal intrinsic brain functional network dynamicsin amnestic mild cognitive impairment
DOI:
https://doi.org/10.71321/bgaxq397Keywords:
aMCI, dynamic functional network, fMRI, multilayer networks, independent component analysis, graph theoryAbstract
Background: Amnestic mild cognitive impairment (aMCI), owing to its high prevalence and significant prognostic relevance for dementia, has become a key focus in the early detection and intervention of neurodegenerative diseases. However, the abnormal intrinsic brain functional network dynamics in aMCI patients remain inadequately understood.
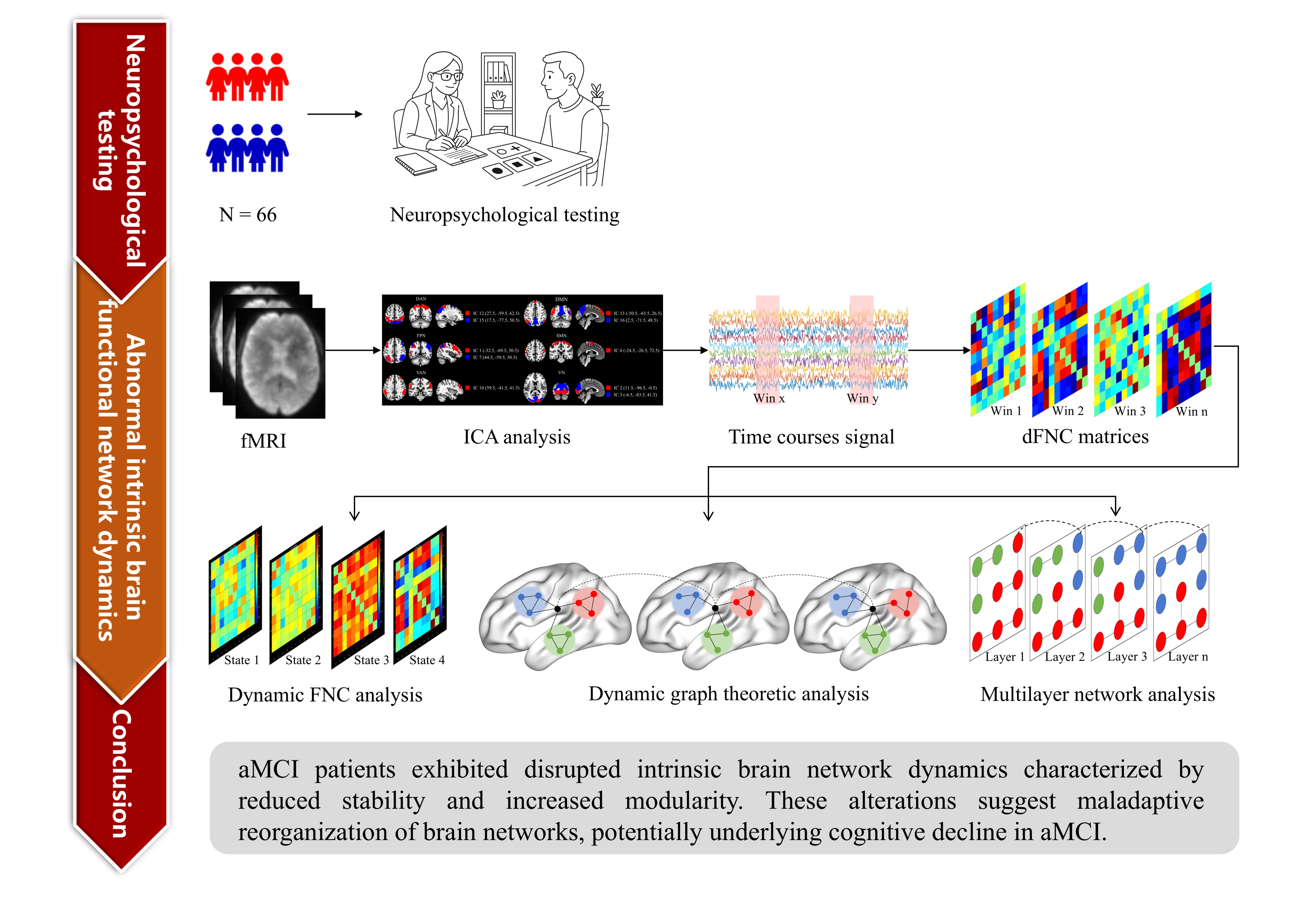
Methods: A total of 66 participants, comprising 31 aMCI patients and 35 age- and education-matched healthy controls (HCs), underwent resting-state fMRI scans and comprehensive neuropsychological assessments. This study examined intrinsic brain network dynamics in aMCI patients via dynamic functional network connectivity (dFNC) analysis, dynamic graph theoretical analysis, and multilayer network analysis.
Results: Compared with HCs, aMCI patients presented a significantly shorter mean dwell time (MDT) in state 2 (P < 0.05). In addition, the modularity coefficient Q was significantly greater in aMCI patients (1.40 ± 1.20) than in HCs (0.90 ± 0.46, P < 0.05). No significant differences were observed between the groups in terms of network efficiency or network switching rates.
Conclusion: These findings emphasize significant abnormal intrinsic brain functional network dynamics in aMCI patients, with disrupted network stability and increased modularity indicating maladaptive reorganization of brain networks. These results provide valuable biomarkers for early diagnosis and intervention, contributing to a deeper understanding of the neurobiological underpinnings of cognitive decline in aMCI patients.
References
[1] Edmonds EC, McDonald CR, Marshall A, Thomas KR, Eppig J, Weigand AJ, et al. (2019). Early versus late MCI: Improved MCI staging using a neuropsychological approach. Alzheimers Dement, 15(5), 699-708. https://doi.org/10.1016/j.jalz.2018.12.009
[2] Gauthier S, Reisberg B, Zaudig M, Petersen RC, Ritchie K, Broich K, et al. (2006). Mild cognitive impairment. Lancet, 367(9518), 1262-1270. https://doi.org/10.1016/s0140-6736(06)68542-5
[3] Mian M, Tahiri J, Eldin R, Altabaa M, Sehar U, & Reddy PH. (2024). Overlooked cases of mild cognitive impairment: Implications to early Alzheimer's disease. Ageing Res Rev, 98, 102335. https://doi.org/10.1016/j.arr.2024.102335
[4] Varela-López B, Zurrón M, Lindín M, Díaz F, & Galdo-Alvarez S. (2025). Compensation versus deterioration across functional networks in amnestic mild cognitive impairment subtypes. Geroscience, 47(2), 1805-1822. https://doi.org/10.1007/s11357-024-01369-9
[5] Golesorkhi M, Gomez-Pilar J, Zilio F, Berberian N, Wolff A, Yagoub MCE, et al. (2021). The brain and its time: intrinsic neural timescales are key for input processing. Commun Biol, 4(1), 970. https://doi.org/10.1038/s42003-021-02483-6
[6] Fu Z, Du Y, & Calhoun VD. (2019). The Dynamic Functional Network Connectivity Analysis Framework. Engineering (Beijing), 5(2), 190-193. https://doi.org/10.1016/j.eng.2018.10.001
[7] Petersen SE, & Sporns O. (2015). Brain Networks and Cognitive Architectures. Neuron, 88(1), 207-219. https://doi.org/10.1016/j.neuron.2015.09.027
[8] Bullmore E, & Sporns O. (2012). The economy of brain network organization. Nat Rev Neurosci, 13(5), 336-349. https://doi.org/10.1038/nrn3214
[9] Sporns O, & Betzel RF. (2016). Modular Brain Networks. Annu Rev Psychol, 67, 613-640. https://doi.org/10.1146/annurev-psych-122414-033634
[10] Chen X, Necus J, Peraza LR, Mehraram R, Wang Y, O'Brien JT, et al. (2021). The functional brain favours segregated modular connectivity at old age unless affected by neurodegeneration. Commun Biol, 4(1), 973. https://doi.org/10.1038/s42003-021-02497-0
[11] Park HJ, & Friston K. (2013). Structural and functional brain networks: from connections to cognition. Science, 342(6158), 1238411. https://doi.org/10.1126/science.1238411
[12] Koch I, Poljac E, Müller H, & Kiesel A. (2018). Cognitive structure, flexibility, and plasticity in human multitasking-An integrative review of dual-task and task-switching research. Psychol Bull, 144(6), 557-583. https://doi.org/10.1037/bul0000144
[13] Bondi MW, Edmonds EC, Jak AJ, Clark LR, Delano-Wood L, McDonald CR, et al. (2014). Neuropsychological criteria for mild cognitive impairment improves diagnostic precision, biomarker associations, and progression rates. J Alzheimers Dis, 42(1), 275-289. https://doi.org/10.3233/jad-140276
[14] Arevalo-Rodriguez I, Smailagic N, Roqué-Figuls M, Ciapponi A, Sanchez-Perez E, Giannakou A, et al. (2021). Mini-Mental State Examination (MMSE) for the early detection of dementia in people with mild cognitive impairment (MCI). Cochrane Database Syst Rev, 7(7), Cd010783. https://doi.org/10.1002/14651858.CD010783.pub3
[15] Li LL, Ma J, Wu JJ, Xue X, Zheng MX, Hua XY, et al. (2025). Impact of effective connectivity within the Papez circuit on episodic memory: moderation by perivascular space function. Alzheimers Res Ther, 17(1), 66. https://doi.org/10.1186/s13195-025-01717-7
[16] Ma J, Zheng MX, Wu JJ, Xing XX, Xiang YT, Wei D, et al. (2023). Mapping the long-term delayed recall-based cortex-hippocampus network constrained by the structural and functional connectome: a case-control multimodal MRI study. Alzheimers Res Ther, 15(1), 61. https://doi.org/10.1186/s13195-023-01197-7
[17] Wilks H, Benzinger TLS, Schindler SE, Cruchaga C, Morris JC, & Hassenstab J. (2024). Predictors and outcomes of fluctuations in the clinical dementia rating scale. Alzheimers Dement, 20(3), 2080-2088. https://doi.org/10.1002/alz.13679
[18] McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR, Jr., Kawas CH, et al. (2011). The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement, 7(3), 263-269. https://doi.org/10.1016/j.jalz.2011.03.005
[19] Chen KL, Xu Y, Chu AQ, Ding D, Liang XN, Nasreddine ZS, et al. (2016). Validation of the Chinese Version of Montreal Cognitive Assessment Basic for Screening Mild Cognitive Impairment. J Am Geriatr Soc, 64(12), e285-e290. https://doi.org/10.1111/jgs.14530
[20] Matias-Guiu JA, Cortés-Martínez A, Valles-Salgado M, Rognoni T, Fernández-Matarrubia M, Moreno-Ramos T, et al. (2017). Addenbrooke's cognitive examination III: diagnostic utility for mild cognitive impairment and dementia and correlation with standardized neuropsychological tests. Int Psychogeriatr, 29(1), 105-113. https://doi.org/10.1017/s1041610216001496
[21] Zhao Q, Guo Q, Liang X, Chen M, Zhou Y, Ding D, et al. (2015). Auditory Verbal Learning Test is Superior to Rey-Osterrieth Complex Figure Memory for Predicting Mild Cognitive Impairment to Alzheimer's Disease. Curr Alzheimer Res, 12(6), 520-526. https://doi.org/10.2174/1567205012666150530202729
[22] Silva PHR, Spedo CT, Baldassarini CR, Benini CD, Ferreira DA, Barreira AA, et al. (2019). Brain functional and effective connectivity underlying the information processing speed assessed by the Symbol Digit Modalities Test. Neuroimage, 184, 761-770. https://doi.org/10.1016/j.neuroimage.2018.09.080
[23] Knesevich JW, LaBarge E, & Edwards D. (1986). Predictive value of the Boston Naming Test in mild senile dementia of the Alzheimer type. Psychiatry Res, 19(2), 155-161. https://doi.org/10.1016/0165-1781(86)90008-9
[24] Zhao Q, Guo Q, & Hong Z. (2013). Clustering and switching during a semantic verbal fluency test contribute to differential diagnosis of cognitive impairment. Neurosci Bull, 29(1), 75-82. https://doi.org/10.1007/s12264-013-1301-7
[25] Chen NC, Chang CC, Lin KN, Huang CW, Chang WN, Chang YT, et al. (2013). Patterns of executive dysfunction in amnestic mild cognitive impairment. Int Psychogeriatr, 25(7), 1181-1189. https://doi.org/10.1017/s1041610213000392
[26] Akkoyun M, Koçoğlu K, Boz HE, Tüfekci IY, Ekin M, Akdal GJAs, et al. (2023). Eye movements during the judgment of line orientation test in patients with Alzheimer’s disease and amnestic mild cognitive impairment. 19, e075697.
[27] Huang L, Chen KL, Lin BY, Tang L, Zhao QH, Li F, et al. (2019). An abbreviated version of Silhouettes test: a brief validated mild cognitive impairment screening tool. Int Psychogeriatr, 31(6), 849-856. https://doi.org/10.1017/s1041610218001230
[28] Calhoun VD, Adali T, Pearlson GD, & Pekar JJ. (2001). A method for making group inferences from functional MRI data using independent component analysis. Hum Brain Mapp, 14(3), 140-151. https://doi.org/10.1002/hbm.1048
[29] Fiorenzato E, Strafella AP, Kim J, Schifano R, Weis L, Antonini A, et al. (2019). Dynamic functional connectivity changes associated with dementia in Parkinson's disease. Brain, 142(9), 2860-2872. https://doi.org/10.1093/brain/awz192
[30] Bell AJ, & Sejnowski TJ. (1995). An information-maximization approach to blind separation and blind deconvolution. Neural Comput, 7(6), 1129-1159. https://doi.org/10.1162/neco.1995.7.6.1129
[31] Himberg J, Hyvärinen A, & Esposito F. (2004). Validating the independent components of neuroimaging time series via clustering and visualization. Neuroimage, 22(3), 1214-1222. https://doi.org/10.1016/j.neuroimage.2004.03.027
[32] Wang D, Qin W, Liu Y, Zhang Y, Jiang T, & Yu C. (2014). Altered resting-state network connectivity in congenital blind. Hum Brain Mapp, 35(6), 2573-2581. https://doi.org/10.1002/hbm.22350
[33] Kim J, Criaud M, Cho SS, Díez-Cirarda M, Mihaescu A, Coakeley S, et al. (2017). Abnormal intrinsic brain functional network dynamics in Parkinson's disease. Brain, 140(11), 2955-2967. https://doi.org/10.1093/brain/awx233
[34] Allen EA, Damaraju E, Plis SM, Erhardt EB, Eichele T, & Calhoun VD. (2014). Tracking whole-brain connectivity dynamics in the resting state. Cereb Cortex, 24(3), 663-676. https://doi.org/10.1093/cercor/bhs352
[35] Lloyd SJItoit. (1982). Least squares quantization in PCM. 28(2), 129-137.
[37] Malhi GS, Das P, Outhred T, Bryant RA, & Calhoun V. (2019). Resting-state neural network disturbances that underpin the emergence of emotional symptoms in adolescent girls: resting-state fMRI study. Br J Psychiatry, 215(3), 545-551. https://doi.org/10.1192/bjp.2019.10
[38] Wang J, Wang X, Xia M, Liao X, Evans A, & He Y. (2015). GRETNA: a graph theoretical network analysis toolbox for imaging connectomics. Front Hum Neurosci, 9, 386. https://doi.org/10.3389/fnhum.2015.00386
[39] Achard S, & Bullmore E. (2007). Efficiency and cost of economical brain functional networks. PLoS Comput Biol, 3(2), e17. https://doi.org/10.1371/journal.pcbi.0030017
[40] Pedersen M, Zalesky A, Omidvarnia A, & Jackson GD. (2018). Multilayer network switching rate predicts brain performance. Proc Natl Acad Sci U S A, 115(52), 13376-13381. https://doi.org/10.1073/pnas.1814785115
[41] Menon V. (2021). Dissociation by Network Integration. Am J Psychiatry, 178(2), 110-112. https://doi.org/10.1176/appi.ajp.2020.20121728
[42] Spreng RN, Stevens WD, Chamberlain JP, Gilmore AW, & Schacter DL. (2010). Default network activity, coupled with the frontoparietal control network, supports goal-directed cognition. Neuroimage, 53(1), 303-317. https://doi.org/10.1016/j.neuroimage.2010.06.016
[43] Hsu CL, Best JR, Voss MW, Handy TC, Beauchet O, Lim C, et al. (2019). Functional Neural Correlates of Slower Gait Among Older Adults With Mild Cognitive Impairment. J Gerontol A Biol Sci Med Sci, 74(4), 513-518. https://doi.org/10.1093/gerona/gly027
[44] Kessler D, Angstadt M, & Sripada C. (2016). Growth Charting of Brain Connectivity Networks and the Identification of Attention Impairment in Youth. JAMA Psychiatry, 73(5), 481-489. https://doi.org/10.1001/jamapsychiatry.2016.0088
[45] Ignatavicius A, Matar E, & Lewis SJG. (2025). Visual hallucinations in Parkinson's disease: spotlight on central cholinergic dysfunction. Brain, 148(2), 376-393. https://doi.org/10.1093/brain/awae289
[46] Li R, Wu X, Fleisher AS, Reiman EM, Chen K, & Yao L. (2012). Attention-related networks in Alzheimer's disease: a resting functional MRI study. Hum Brain Mapp, 33(5), 1076-1088. https://doi.org/10.1002/hbm.21269
[47] Pini L, de Lange SC, Pizzini FB, Boscolo Galazzo I, Manenti R, Cotelli M, et al. (2022). A low-dimensional cognitive-network space in Alzheimer's disease and frontotemporal dementia. Alzheimers Res Ther, 14(1), 199. https://doi.org/10.1186/s13195-022-01145-x
[48] Bertolero MA, Yeo BT, & D'Esposito M. (2015). The modular and integrative functional architecture of the human brain. Proc Natl Acad Sci U S A, 112(49), E6798-6807. https://doi.org/10.1073/pnas.1510619112
[49] Baum GL, Ciric R, Roalf DR, Betzel RF, Moore TM, Shinohara RT, et al. (2017). Modular Segregation of Structural Brain Networks Supports the Development of Executive Function in Youth. Curr Biol, 27(11), 1561-1572.e1568. https://doi.org/10.1016/j.cub.2017.04.051
[50] Avena-Koenigsberger A, Misic B, & Sporns O. (2017). Communication dynamics in complex brain networks. Nat Rev Neurosci, 19(1), 17-33. https://doi.org/10.1038/nrn.2017.149
Type
Published
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material; further inquiries can be directed to the corresponding author.
Issue
Section
License
Copyright (c) 2025 Brain Conflux

This work is licensed under a Creative Commons Attribution 4.0 International License.







