Causal Relationships between 1400 Serum Metabolite Traits,179 Plasma Lipids, and Hemorrhoids: A Mendelian Randomization Study and Meta-analysis
DOI:
https://doi.org/10.71321/8s70we60Keywords:
Serum Metabolites, Plasma Lipids, Hemorrhoids, Mendelian Randomization, Meta-analysisAbstract
Background: Hemorrhoids is a common anorectal disorder that significantly impacts patients' quality of life over the long term and imposes a substantial economic burden. However, the potential link between HD and serum metabolites and lipids has been scarcely studied, and its pathogenesis remains unclear.
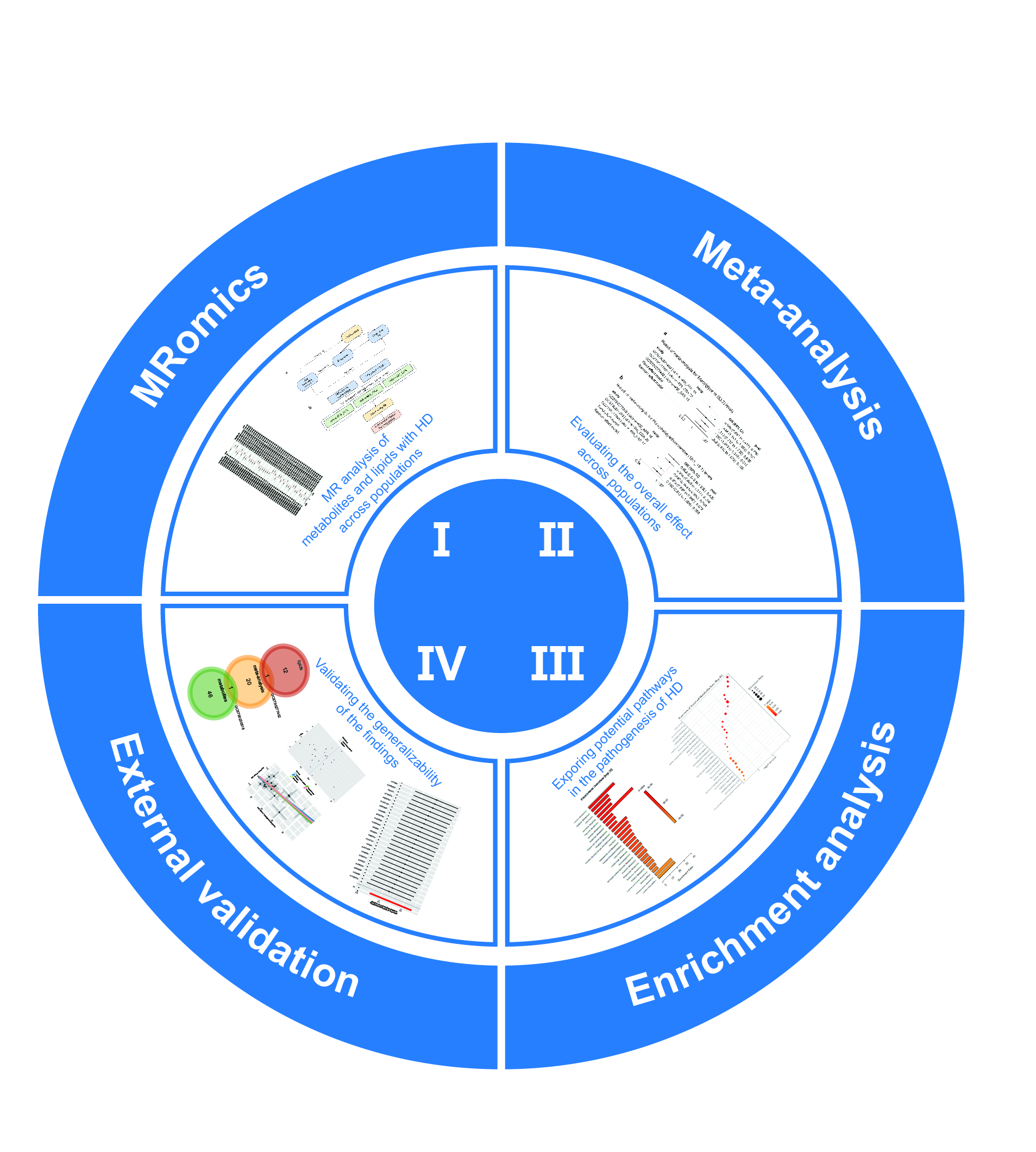
Methods: The causal relationships between serum metabolite traits, plasma lipids, and HD were evaluated using Mendelian Randomization. Inverse Variance Weighted was the most important analysis approach. Sensitivity analysis was used to assess the robustness of the results. Enrichment analysis was applied to the metabolites obtained from the results of MR analysis and meta-analysis.
Results: The risk factors included Citramalate levels (OR = 1.487, 95%CI = 1.172-1.888, P = 0.001), P-cresol sulfate levels (OR = 1.476, 95%CI = 1.111-1.961, P = 0.007), and Triacylglycerol (53:3) levels (OR = 1.262, 95%CI = 1.049-1.518, P = 0.014). The protective factors included Imidazole lactate levels (OR = 0.865, 95%CI = 0.756-0.989, P = 0.034), 1-(1-enyl-stearoyl)-GPE (p-18:0) levels (OR = 0.722, 95%CI = 0.552-0.944, P = 0.017), and Phosphatidylethanolamine (18:1_18:1) levels (OR = 0.803, 95%CI = 0.666-0.969, P = 0.022). Enrichment analysis showed that risk factors were enriched in Alanine Metabolism (Holm P = 0.0039), Cysteine Metabolism (Holm P = 0.0146), Urea Cycle (Holm P = 0.0181), and Ammonia Recycling (Holm P = 0.0245). Protective factors were enriched in the Urea Cycle (Holm P = 0.00754), Ammonia Recycling (Holm P = 0.0102), Aspartate Metabolism (Holm P = 0.0147), Glutamate Metabolism (Holm P = 0.038), Arginine and Proline Metabolism (Holm P = 0.0479), and Malate-Aspartate Shuttle (Holm P = 0.0495).
Conclusion: Previous studies often focused on the causal relationships between a few potential risk factors and HD in a single population. Our study is the first to address this gap by integrating a broad range of 1400 metabolites and 179 lipids with HD across diverse populations, and identifying specific metabolic pathways involved in HD development.
References
[1] Agarwal N, Singh K, Sheikh P, Mittal K, Mathai V, & Kumar A. (2017). Executive Summary - The Association of Colon & Rectal Surgeons of India (ACRSI) Practice Guidelines for the Management of Haemorrhoids-2016. Indian J Surg, 79(1), 58-61. https://doi.org/10.1007/s12262-016-1578-7
[2] Wu EB, Sung FC, Lin CL, Wu KL, & Chen KB. (2021). Colorectal Cancer Risk in Patients with Hemorrhoids: A 10-Year Population-Based Retrospective Cohort Study. Int J Environ Res Public Health, 18(16). https://doi.org/10.3390/ijerph18168655
[3] Pata F, Sgró A, Ferrara F, Vigorita V, Gallo G, & Pellino G. (2021). Anatomy, Physiology and Pathophysiology of Haemorrhoids. Rev Recent Clin Trials, 16(1), 75-80. https://doi.org/10.2174/1574887115666200406115150
[4] Zheng T, Ellinghaus D, Juzenas S, Cossais F, Burmeister G, Mayr G, et al. (2021). Genome-wide analysis of 944 133 individuals provides insights into the etiology of haemorrhoidal disease. Gut, 70(8), 1538-1549. https://doi.org/10.1136/gutjnl-2020-323868
[5] Vijayvargiya P, Camilleri M, Carlson P, Lueke A, O'Neill J, Burton D, et al. (2017). Performance characteristics of serum C4 and FGF19 measurements to exclude the diagnosis of bile acid diarrhoea in IBS-diarrhoea and functional diarrhoea. Aliment Pharmacol Ther, 46(6), 581-588. https://doi.org/10.1111/apt.14214
[6] Zhao R, Zhang Q, Huang T, Tian Y, Guan G, & Lin Y. (2024). Effect of the Combination of Clostridium butyricum and Mycelium of Phellinus igniarius on Intestinal Microbiota and Serum Metabolites in DSS-Induced Colitis. Nutrients, 16(1). https://doi.org/10.3390/nu16010153
[7] Chen F, Dai X, Zhou CC, Li KX, Zhang YJ, Lou XY, et al. (2022). Integrated analysis of the faecal metagenome and serum metabolome reveals the role of gut microbiome-associated metabolites in the detection of colorectal cancer and adenoma. Gut, 71(7), 1315-1325. https://doi.org/10.1136/gutjnl-2020-323476
[8] Liu R, Hong J, Xu X, Feng Q, Zhang D, Gu Y, et al. (2017). Gut microbiome and serum metabolome alterations in obesity and after weight-loss intervention. Nat Med, 23(7), 859-868. https://doi.org/10.1038/nm.4358
[9] Yu M, Shang Y, Han L, & Yu X. (2024). Bowel Habits, Obesity, Intestinal Microbiota and Their Influence on Hemorrhoidal Disease: a Mendelian Randomization Study. Clin Exp Gastroenterol, 17, 157-164. https://doi.org/10.2147/ceg.S450807
[10] Han X, & Gross RW. (2022). The foundations and development of lipidomics. J Lipid Res, 63(2), 100164. https://doi.org/10.1016/j.jlr.2021.100164
[11] Yoon H, Shaw JL, Haigis MC, & Greka A. (2021). Lipid metabolism in sickness and in health: Emerging regulators of lipotoxicity. Mol Cell, 81(18), 3708-3730. https://doi.org/10.1016/j.molcel.2021.08.027
[12] Zeng C, Wen B, Hou G, Lei L, Mei Z, Jia X, et al. (2017). Lipidomics profiling reveals the role of glycerophospholipid metabolism in psoriasis. Gigascience, 6(10), 1-11. https://doi.org/10.1093/gigascience/gix087
[13] Nowowiejska J, Baran A, & Flisiak I. (2023). Lipid Alterations and Metabolism Disturbances in Selected Inflammatory Skin Diseases. Int J Mol Sci, 24(8). https://doi.org/10.3390/ijms24087053
[14] Szmitko PE, Wang CH, Weisel RD, Jeffries GA, Anderson TJ, & Verma S. (2003). Biomarkers of vascular disease linking inflammation to endothelial activation: Part II. Circulation, 108(17), 2041-2048. https://doi.org/10.1161/01.Cir.0000089093.75585.98
[15] Wang R, Zhang Y, Xu L, Lin Y, Yang X, Bai L, et al. (2016). Protein Inhibitor of Activated STAT3 Suppresses Oxidized LDL-induced Cell Responses during Atherosclerosis in Apolipoprotein E-deficient Mice. Sci Rep, 6, 36790. https://doi.org/10.1038/srep36790
[16] Aron-Wisnewsky J, Warmbrunn MV, Nieuwdorp M, & Clément K. (2021). Metabolism and Metabolic Disorders and the Microbiome: The Intestinal Microbiota Associated With Obesity, Lipid Metabolism, and Metabolic Health-Pathophysiology and Therapeutic Strategies. Gastroenterology, 160(2), 573-599. https://doi.org/10.1053/j.gastro.2020.10.057
[17] Kattar SA, Jurjus R, Pinon A, Leger DY, Jurjus A, Boukarim C, et al. (2020). Metformin and Probiotics in the Crosstalk between Colitis-Associated Colorectal Cancer and Diabetes in Mice. Cancers (Basel), 12(7). https://doi.org/10.3390/cancers12071857
[18] Huang J, Gui Y, Qin H, & Xie Y. (2023). Causal association between adiposity and hemorrhoids: a Mendelian randomization study. Front Med (Lausanne), 10, 1229925. https://doi.org/10.3389/fmed.2023.1229925
[19] Wang Z, Yang M, Shi R, & Wang J. (2024). Association between low-density lipoprotein and hemorrhoids in east Asian populations: A multivariate Mendelian randomization study. Asian J Surg, 47(10), 4514-4515. https://doi.org/10.1016/j.asjsur.2024.07.230
[20] Lawlor DA, Harbord RM, Sterne JA, Timpson N, & Davey Smith G. (2008). Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med, 27(8), 1133-1163. https://doi.org/10.1002/sim.3034
[21] Chen Y, Lu T, Pettersson-Kymmer U, Stewart ID, Butler-Laporte G, Nakanishi T, et al. (2023). Genomic atlas of the plasma metabolome prioritizes metabolites implicated in human diseases. Nat Genet, 55(1), 44-53. https://doi.org/10.1038/s41588-022-01270-1
[22] Ottensmann L, Tabassum R, Ruotsalainen SE, Gerl MJ, Klose C, Widén E, et al. (2023). Genome-wide association analysis of plasma lipidome identifies 495 genetic associations. Nat Commun, 14(1), 6934. https://doi.org/10.1038/s41467-023-42532-8
[24] Bowden J, Davey Smith G, & Burgess S. (2015). Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol, 44(2), 512-525. https://doi.org/10.1093/ije/dyv080
[26] Hemani G, Bowden J, & Davey Smith G. (2018). Evaluating the potential role of pleiotropy in Mendelian randomization studies. Hum Mol Genet, 27(R2), R195-r208. https://doi.org/10.1093/hmg/ddy163
[28] Li Y, Nicholson RJ, & Summers SA. (2022). Ceramide signaling in the gut. Mol Cell Endocrinol, 544, 111554. https://doi.org/10.1016/j.mce.2022.111554
[29] Yu S, Sun Y, Shao X, Zhou Y, Yu Y, Kuai X, et al. (2022). Leaky Gut in IBD: Intestinal Barrier-Gut Microbiota Interaction. J Microbiol Biotechnol, 32(7), 825-834. https://doi.org/10.4014/jmb.2203.03022
[30] Jain AP, Aggarwal KK, & Zhang PY. (2015). Omega-3 fatty acids and cardiovascular disease. Eur Rev Med Pharmacol Sci, 19(3), 441-445.
[31] D'Souza BN, Yadav M, Chaudhary PP, Ratley G, Lu MY, Alves DA, et al. (2024). Derivation of novel metabolic pathway score identifies alanine metabolism as a targetable influencer of TNF-alpha signaling. Heliyon, 10(13), e33502. https://doi.org/10.1016/j.heliyon.2024.e33502
[32] Chen X, Xun K, Chen L, & Wang Y. (2009). TNF-alpha, a potent lipid metabolism regulator. Cell Biochem Funct, 27(7), 407-416. https://doi.org/10.1002/cbf.1596
[33] Tiwary SK, Kumar A, Mishra SP, Kumar P, & Khanna AK. (2020). Study of association of varicose veins and inflammation by inflammatory markers. Phlebology, 35(9), 679-685. https://doi.org/10.1177/0268355520932410
[34] Jacob MP. (2003). Extracellular matrix remodeling and matrix metalloproteinases in the vascular wall during aging and in pathological conditions. Biomed Pharmacother, 57(5-6), 195-202. https://doi.org/10.1016/s0753-3322(03)00065-9
[35] Mannello F, & Raffetto JD. (2011). Matrix metalloproteinase activity and glycosaminoglycans in chronic venous disease: the linkage among cell biology, pathology and translational research. Am J Transl Res, 3(2), 149-158.
[36] Raffetto JD, & Khalil RA. (2021). Mechanisms of Lower Extremity Vein Dysfunction in Chronic Venous Disease and Implications in Management of Varicose Veins. Vessel Plus, 5. https://doi.org/10.20517/2574-1209.2021.16
[37] Kucukguven A, & Khalil RA. (2013). Matrix metalloproteinases as potential targets in the venous dilation associated with varicose veins. Curr Drug Targets, 14(3), 287-324.
[38] MacColl E, & Khalil RA. (2015). Matrix Metalloproteinases as Regulators of Vein Structure and Function: Implications in Chronic Venous Disease. J Pharmacol Exp Ther, 355(3), 410-428. https://doi.org/10.1124/jpet.115.227330
[39] Bierhansl L, Conradi LC, Treps L, Dewerchin M, & Carmeliet P. (2017). Central Role of Metabolism in Endothelial Cell Function and Vascular Disease. Physiology (Bethesda), 32(2), 126-140. https://doi.org/10.1152/physiol.00031.2016
[40] Sabbatinelli J, Prattichizzo F, Olivieri F, Procopio AD, Rippo MR, & Giuliani A. (2019). Where Metabolism Meets Senescence: Focus on Endothelial Cells. Front Physiol, 10, 1523. https://doi.org/10.3389/fphys.2019.01523
[41] Sharp CD, Houghton J, Elrod JW, Warren A, Jackson THt, Jawahar A, et al. (2005). N-methyl-D-aspartate receptor activation in human cerebral endothelium promotes intracellular oxidant stress. Am J Physiol Heart Circ Physiol, 288(4), H1893-1899. https://doi.org/10.1152/ajpheart.01110.2003
[42] Tao Q, Ma N, Fan L, Ge W, Zhang Z, Liu X, et al. (2024). Multi-Omics Approaches for Liver Reveal the Thromboprophylaxis Mechanism of Aspirin Eugenol Ester in Rat Thrombosis Model. Int J Mol Sci, 25(4). https://doi.org/10.3390/ijms25042141
[43] Chatterjee M, Ehrenberg A, Toska LM, Metz LM, Klier M, Krueger I, et al. (2020). Molecular Drivers of Platelet Activation: Unraveling Novel Targets for Anti-Thrombotic and Anti-Thrombo-Inflammatory Therapy. Int J Mol Sci, 21(21). https://doi.org/10.3390/ijms21217906
[44] Lee NT, Ong LK, Gyawali P, Nassir C, Mustapha M, Nandurkar HH, et al. (2021). Role of Purinergic Signalling in Endothelial Dysfunction and Thrombo-Inflammation in Ischaemic Stroke and Cerebral Small Vessel Disease. Biomolecules, 11(7). https://doi.org/10.3390/biom11070994
[45] Li Y, Li R, Feng Z, Wan Q, & Wu J. (2020). Linagliptin Regulates the Mitochondrial Respiratory Reserve to Alter Platelet Activation and Arterial Thrombosis. Front Pharmacol, 11, 585612. https://doi.org/10.3389/fphar.2020.585612
[46] Grisham MB, Jourd'Heuil D, & Wink DA. (1999). Nitric oxide. I. Physiological chemistry of nitric oxide and its metabolites:implications in inflammation. Am J Physiol, 276(2), G315-321. https://doi.org/10.1152/ajpgi.1999.276.2.G315
[47] Phang JM, Liu W, & Zabirnyk O. (2010). Proline metabolism and microenvironmental stress. Annu Rev Nutr, 30, 441-463. https://doi.org/10.1146/annurev.nutr.012809.104638
[48] Ying W, & Xiong ZG. (2010). Oxidative stress and NAD+ in ischemic brain injury: current advances and future perspectives. Curr Med Chem, 17(20), 2152-2158. https://doi.org/10.2174/092986710791299911
[49] Chen H, Wang C, Wei X, Ding X, & Ying W. (2015). Malate-Aspartate Shuttle Inhibitor Aminooxyacetate Acid Induces Apoptosis and Impairs Energy Metabolism of Both Resting Microglia and LPS-Activated Microglia. Neurochem Res, 40(6), 1311-1318. https://doi.org/10.1007/s11064-015-1589-y
[50] Walker V. (2009). Ammonia toxicity and its prevention in inherited defects of the urea cycle. Diabetes Obes Metab, 11(9), 823-835. https://doi.org/10.1111/j.1463-1326.2009.01054.x
[51] Matsumoto S, Häberle J, Kido J, Mitsubuchi H, Endo F, & Nakamura K. (2019). Urea cycle disorders-update. J Hum Genet, 64(9), 833-847. https://doi.org/10.1038/s10038-019-0614-4
[52] Abdoun K, Stumpff F, & Martens H. (2006). Ammonia and urea transport across the rumen epithelium: a review. Anim Health Res Rev, 7(1-2), 43-59. https://doi.org/10.1017/s1466252307001156
[53] Walker V. (2014). Ammonia metabolism and hyperammonemic disorders. Adv Clin Chem, 67, 73-150. https://doi.org/10.1016/bs.acc.2014.09.002
[54] Ferrario M, Pastorelli R, Brunelli L, Liu S, Zanella do Amaral Campos PP, Casoni D, et al. (2021). Persistent hyperammonia and altered concentrations of urea cycle metabolites in a 5-day swine experiment of sepsis. Sci Rep, 11(1), 18430. https://doi.org/10.1038/s41598-021-97855-7
[55] Aldridge DR, Tranah EJ, & Shawcross DL. (2015). Pathogenesis of hepatic encephalopathy: role of ammonia and systemic inflammation. J Clin Exp Hepatol, 5(Suppl 1), S7-s20. https://doi.org/10.1016/j.jceh.2014.06.004
[56] Fu A, Alvarez-Perez JC, Avizonis D, Kin T, Ficarro SB, Choi DW, et al. (2020). Glucose-dependent partitioning of arginine to the urea cycle protects β-cells from inflammation. Nat Metab, 2(5), 432-446. https://doi.org/10.1038/s42255-020-0199-4
[57] Rojas Á, García-Lozano MR, Gil-Gómez A, Romero-Gómez M, & Ampuero J. (2022). Glutaminolysis-ammonia-urea Cycle Axis, Non-alcoholic Fatty Liver Disease Progression and Development of Novel Therapies. J Clin Transl Hepatol, 10(2), 356-362. https://doi.org/10.14218/jcth.2021.00247
[58] Vayá A, Falcó C, Simó M, Ferrando F, Mira Y, Todolí J, et al. (2007). Influence of lipids and obesity on haemorheological parameters in patients with deep vein thrombosis. Thromb Haemost, 98(3), 621-626.
[59] Saghazadeh A, Hafizi S, & Rezaei N. (2015). Inflammation in venous thromboembolism: Cause or consequence? Int Immunopharmacol, 28(1), 655-665. https://doi.org/10.1016/j.intimp.2015.07.044
[60] Poredos P, Spirkoska A, Rucigaj T, Fareed J, & Jezovnik MK. (2015). Do blood constituents in varicose veins differ from the systemic blood constituents? Eur J Vasc Endovasc Surg, 50(2), 250-256. https://doi.org/10.1016/j.ejvs.2015.04.031
Type
Published
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding authors.
Issue
Section
License
Copyright (c) 2025 Life Conflux

This work is licensed under a Creative Commons Attribution 4.0 International License.







